How Could Stem Cells Cure Blindness? Experts Discuss Their Investigational Stem Cell Therapy to Restore Vision
News VideoPeople over the age of 75 have nearly a 30% risk of developing age-related macular degeneration (AMD), which now affects 11 million in the United States. These patients experience a loss of central vision that can make daily life a struggle.
NYSCF is developing a cell therapy to restore vision in AMD patients using their own stem cells by leveraging technology pioneered by scientists at the National Eye Institute (NEI) in partnership with surgeons at Columbia University. The experts behind this investigational therapy recently gathered to give an update on its path to the clinic.
What causes AMD and how is it currently treated?
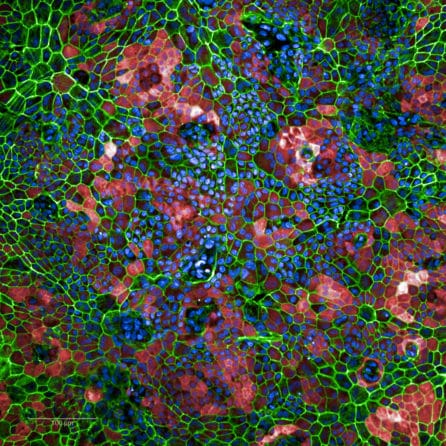
“The vision loss that happens in AMD results from a loss of photoreceptor cells: those that perceive light and send signals to the brain,” explained Kapil Bharti, PhD, of the National Eye Institute, who has pioneered methods for creating the cells that will be used in the transplant. “The reason photoreceptors die is because adjacent to them lives a group called ‘retinal pigmented epithelial cells’ or RPE cells, and in AMD, death of RPE cells leads to loss of photoreceptors, and in turn, blindness.”
Treatment options depend on which form of AMD a patient has: wet or dry.
“Early AMD starts with little deposits called drusen in the back of the eye where the RPE cells live,” explained Stanley Chang, MD, of Columbia University, whose team will carry out the transplants. “As we get older, drusen increases and RPE cells die. And this can lead to dry AMD, which accounts for about 80-90% of AMD cases. The other form, wet AMD, occurs when blood vessels bleed and damage the retina.”
While there are well-established treatments for wet AMD, there aren’t any options for dry AMD that can stop or reverse the disease – that’s where cell therapies come in.
How will NYSCF’s cell therapy work?
“If we can replace diseased cells, that means we’re really going for a cure in which patients won’t have to continue taking a drug or receiving repeated treatments,” noted Howard Kim, PhD, who leads NYSCF’s cell therapy program for AMD.
“Our work builds off that of that of 2011 NYSCF – Robertson Stem Cell Prize Recipient Peter Coffey, DPhil, who created RPE cells from embryonic stem cells and was able to restore vision in AMD patients in early clinical trials,” added NYSCF’s Raeka Aiyar, PhD, who moderated the discussion. “Our work uses induced pluripotent stem cells, meaning they come from the patient themselves, and this will hopefully reduce the risk of immune rejection.”
“When you get a transplant of someone else’s cells, there’s always risk of immune rejection, so you have to take medications to prevent this,” noted Dr. Chang. “With induced pluripotent stem cells from a patient themself, however, immune rejection shouldn’t be a problem since the body won’t recognize them as foreign.”
The process of creating these cells starts with a standard blood draw. Scientists at NYSCF use advanced techniques to turn blood into induced pluripotent stem cells – an approximately 3-month process.
“Then, to turn stem cells into RPE cells, we use a recipe developed by Kapil’s team at NEI that takes about two and a half months,” added NYSCF’s Cecile Terrenoire, PhD, who leads NYSCF’s process development. “We can take about one million stem cells, put them in a petri dish and feed them a kind of ‘cell soup’ that has chemicals, vitamins, and growth factors that mimic the development that naturally occurs in the body.”
“Then, we put the RPE cells into a special patch that is smaller than a tic tac, and that is transplanted into the back of the eye, where the cells will integrate and hopefully restore vision.”
What does it take to bring a cell therapy out of the lab and into the clinic?
“Cell therapies, like any kind of treatment, have to go through the FDA for approval, then into clinical trials before becoming broadly available,” explained Dr. Kim. “The challenge here is that it’s a living drug. Typically, a drug is a chemical that is very stable and easy to analyze. Cells, however, are living things: they change, they can’t – for lack of a better term – be sterilized. So it’s a bigger challenge.”
All the cells used in the transplant are created in NYSCF’s good manufacturing practices (GMP) suite: a specialized clean room for producing clinical-grade cells.
“We’ve built our GMP facility and have done a technology transfer with Kapil to leverage his protocol [for creating RPE cells], which is a formal, documented process. Finally, on the regulatory side, we’ve had what they call a pre-IND meeting with the FDA where we presented our preliminary data and received feedback on next steps. So we’re just going through the final checks and balances with the FDA before we formally submit for approval to initiate our clinical trial.”
What is the status of Dr. Bharti’s AMD trial with the National Eye Institute?
The NYSCF therapy leverages technology developed by Dr. Bharti, who is currently conducting his own AMD trial.
“The trial was approved right before the pandemic and we had to shut it down, but we’re back in swing now,” he said. “We transplanted the first patient last August, and we’re now in the process of enrolling additional patients. This is still considered a safety and feasibility study, so we’ll have more to report after the one year mark when we follow up with patients.”
Enrollment information for this trial can be found here.
Why is it important to have NYSCF’s trial as a complement to this work?
“The aim is to broaden access to this exciting novel treatment,” said Dr. Kim. “The more people working on this, the more data we’ll have, and the more patients can be provided with this treatment in the short and long term.”
“Another point to consider is that once the cells are made, the transplant has to happen somewhere that is within driving distance of the lab – the cells cannot be shipped,” added Dr. Terrenoire. “There’s a high demand everywhere in the country for a treatment like this, so the more geographic locations where the trial can take place, the more people that can be treated.”
Can you give some insight into how this collaboration works?
“We had to get creative during the pandemic,” said Dr. Bharti. “So when we did the technology transfer to NYSCF, we were hoping that teams would go back and forth and learn from each other’s expertise, but we had to make videos of key activities instead to send to Cecile and Howard. Then they would make their own video of what they learned and send it back to us for review.”
Despite the hurdles of COVID, the panelists agreed that this has been an especially rewarding collaboration.
“It’s been a truly amazing and wonderful collaboration,” remarked Dr. Terrenoire. “I’ve been a part of many collaborations before, but this one has stood out as working especially well.”
The team also highlighted that none of this would be possible without the visionary leadership of NYSCF’s Founding CEO Susan L. Solomon, JD, who passed away last fall.
“I’d like to give credit to Susan Solomon who had the foresight to really initiate this collaboration,” said Dr. Chang. “Unfortunately Susan is not going to see the fruits of all her hard work, but we really should give her all the credit for bringing us together.”
Who will be eligible for NYSCF’s trial?
“In general, phase one trials are aimed at evaluating safety, so we often turn to people with more advanced disease – in this case, likely vision range of 20/100 or worse,” said Dr. Kim. “Because with people who have later stage disease, potential complications likely won’t do as much damage as they would in someone with relatively good vision at the moment.”
“We’re anticipating that we will launch the trial mid-next year, so we will announce information about enrollment when that time comes.”
Once a patient receives the transplant, how long will it take to work?
The team cannot say for sure how quickly the transplant could confer results, as that is part of what the trial will assess, but patients will be closely monitored and will hopefully see gradual improvement over time.
“We would follow up one year after the transplant to evaluate whether the patient’s vision has improved, although after a few months we would likely have an idea of how the surgery went,” said Dr. Chang. “These healthy cells may also rejuvenate some of the surrounding cells that have begun to decline in function. These are all things we would monitor.”
Why are you optimistic about this therapy and other cell therapies in the future?
All of the panelists look forward to the results of this trial as well as what it will mean for other diseases.
“We have an opportunity to save a lot of people from being severely blind and keep them functioning, which is our goal,” remarked Dr. Chang. “We want to keep them working, reading, driving, seeing their loved ones.”
“What we’re doing here, hopefully, is laying the groundwork for future therapies that can include other cell types to treat other conditions like glaucoma or even optic neuritis,” he continued.
“Even beyond the eye, there’s a lot of potential. At NYSCF, we can turn stem cells into many different cell types, and so I think the work we’re doing right now with making clinical-grade cells can be applied to other disease areas too as we work toward developing more cell therapies,” said Dr. Terrenoire.
“I think we are going to see a lot coming out of this space in the next several years,” added Dr. Bharti. “It’s exciting times, and I think induced pluripotent stem cell therapies are going to lead the way.”

