Hidden Signatures of Parkinson’s Disease Revealed by NYSCF’s Automation Technology and Artificial Intelligence
The Context: The vast majority of drugs fail clinical trials, largely because there is still much we do not...
About Parkinson's Disease Parkinson's Disease News Publications FAQs Participate in Research
At NYSCF, we are studying the actual human brain cells implicated in the disease to develop novel Parkinson’s treatments. We are doing this in several steps:
Learn more about participating in research at NYSCF.
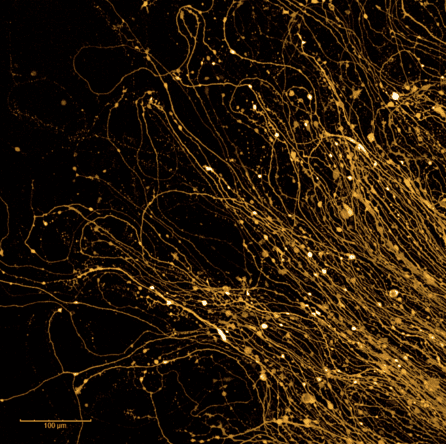
Parkinson’s disease is a chronic, progressive, neurodegenerative disorder that affects over one million Americans and ten million people worldwide, including over 1% of people over the age of 60. The disease stems from dysfunction and deterioration of brain cells, mainly dopamine-producing neurons.
The main motor symptoms of Parkinson’s are tremors, rigidity, slowness of movement, and impaired balance or coordination. A plethora of other debilitating symptoms are often observed, including depression, anxiety, irritability, insomnia, constipation, impulse control disorders, pain, fatigue, and vision problems.
The information provided is not medical advice and is not intended to be medical advice. If you are experiencing any of these symptoms, please talk to your doctor to determine the best course of action for your situation.
While decades of research has begun to reveal genetic and biological factors that contribute to Parkinson’s disease, the precise mechanisms are not known yet, and there are no current treatments to change the disease course, only symptom management approaches.
A Parkinson’s disease diagnosis cannot be determined by a single test but is rather assigned based on a patient’s medical history, symptoms, and a series of neurological and physical exams. Each patient’s Parkinson’s disease prognosis is different, as the disease is unique to each person. While all patients will experience some degree of motor dysfunction, the severity and course that the disease takes may differ from person to person.
The Context: The vast majority of drugs fail clinical trials, largely because there is still much we do not...
How is artificial intelligence (AI) augmenting and improving disease research? A group representing several facets of the disease experience...
Why do some people develop Parkinson’s disease (PD) while others do not? The answer involves a complex interplay between...
A multi-institutional team of scientists led by Lorenz Studer, MD (Memorial Sloan Kettering Cancer Center) and including Gist Croft,...
Below are select publications on recent advancements in Parkinson’s research by NYSCF Research Institute scientists.
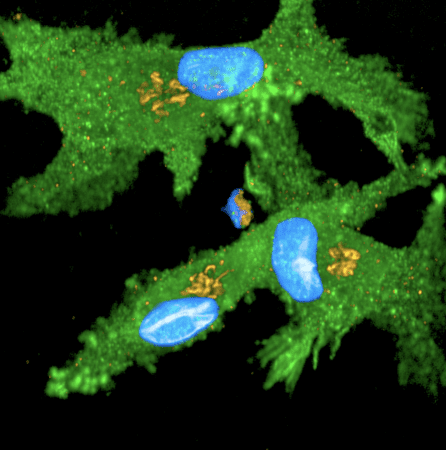
CD49f is a novel marker of functional and reactive human iPSC-derived astrocytes
Lilianne Barbar, Tanya Jain, Matthew Zimmer, Ilya Kruglikov, Jessica Sadick, Minghui Wang, Kriti Kalpana, Indigo V.L. Rose, Suzanne R. Burstein, Tomasz Rusielewicz, Madhura Nijsure, Kevin A Guttenplan, Angelique di Domenico, Gist Croft, Bin Zhang, Hiroko Nobuta, Jean M. Hébert, Shane A. Liddelow, Valentina Fossati. Neuron. 2020. DOI: https://doi.org/10.1016/j.neuron.2020.05.014
This study creates astrocytes – an integral support cell in the brain – from stem cells and shows that in disease-like environments, these normally helpful cells can turn into neuron-killers.
Directed differentiation of human pluripotent stem cells to microglia.
Douvaras P, Sun B, Wang M, Kruglikov I, Lallos G, Zimmer M, Terrenoire C, Zhang B, Gandy S, Schadt E, Freytes DO, Noggle S, Fossati V.
Stem Cell Reports. 2017. doi: 10.1016/j.stemcr.2017.04.023.
In this study, NYSCF researchers developed a protocol for turning stem cells into microglia (the immune cells of the brain). Microglia have recently been implicated in PD, and having an effective method to generate them will allow scientists to elucidate their precise role in the disease.
iPSC-derived dopamine neurons reveal differences between monozygotic twins discordant for Parkinson’s disease.
Woodard CM, Campos BA, Kuo SH, Nirenberg MJ, Nestor MW, Zimmer M, Mosharov EV, Sulzer D, Zhou H, Paull D, Clark L, Schadt EE, Sardi SP, Rubin L, Eggan K, Brock M, Lipnick S, Rao M, Chang S, Li A, Noggle SA.
Cell Reports. 2014. doi: 10.1016/j.celrep.2014.10.023.
In this study, NYSCF scientists derived stem cells and then dopamine neurons from a genetically identical set of twins (one with Parkinson’s disease and one without). This revealed unexpected molecular differences between the twins’ cell lines that indicate which genetic and environmental factors may trigger Parkinson’s onset.
About 10% of Parkinson’s cases have been linked to genetics. Most cases are non-familial (are not accompanied by a genetic mutation). There are several genetic mutations known to be associated with increased risk for developing Parkinson’s, but not all people with these mutations will get the disease.
The most common medication for Parkinson’s disease is levodopa (L-dopa). L-dopa is a precursor to dopamine, the neurotransmitter that is depleted in Parkinson’s. This medication can only help with symptoms and does not stop or cure the disease. Current medications are also limited by serious side effects such as hallucinations, cognitive deficits, dizziness, sleepiness, and compulsive behaviors. At NYSCF, we are committed to finding safe and effective therapies that will do more than mask Parkinson’s disease symptoms, instead targeting the root of the disease.
Our research would not be possible without volunteers who participate in our studies. Learn more about participating in clinical research at NYSCF.