COVID-19 Vaccines Are Finally Here: Experts Discuss How to Distribute Them Efficiently and Ethically
News VideoAfter a long 10 months, COVID-19 vaccines are finally here. The next obstacle? Determining how to distribute them efficiently, ethically, and economically.
Last week, experts in medicine, research, economics, and ethics joined us for a panel discussion about how we can best allocate vaccines and ensure that all communities can benefit from them.
This discussion was moderated by NYSCF Associate Vice President of Scientific Outreach Raeka Aiyar, PhD, and featured Jeffrey Kahn, PhD, MPH (Andreas C. Dracopoulos Director, The Berman Institute for Bioethics, Johns Hopkins University), Valerie Montgomery Rice, MD, FACOG (President and Dean, Morehouse School of Medicine), Daniel Polsky, PhD (Bloomberg Distinguished Professor of Health Economics, Johns Hopkins University), and Susan L. Solomon, JD (CEO and Founder, The NYSCF Research Institute).
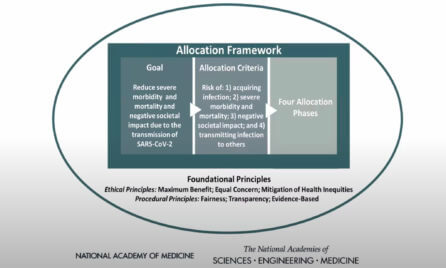
To help prioritize the vaccine rollout across different groups, a National Academies of Sciences, Engineering, and Medicine (NASEM) committee that included Dr. Polsky developed a framework released in October. That framework was then used by the CDC to develop more specific guidelines, which states are now implementing on their own to vaccinate the population in tiers.
“The goal here was to reduce severity, severe morbidity and mortality, and the negative societal impact due to the transmission SARS-CoV-2,” Dr. Polsky said of the framework. “It’s going to take a long time for there to be enough doses manufactured, and to get them to everyone who needs them. So, who goes first? In our recommendations, we had a jumpstart phase that includes high-risk health workers and first responders followed by people of all ages with co-morbid and underlying conditions, and then older adults living in congregate or overcrowded settings.”
Ethics: How Do We Prioritize Vaccine Distribution?
Nearly every aspect of the vaccine rollout poses a question about ethics, and Dr. Kahn noted several areas in which this issue is most apparent.
“What do we owe to the public as a matter of health, and what resources need to be invested to make sure that they’re protected?” he posited. “Each state has a somewhat different framework, which means that if you live in a different place, you may actually see your vaccine sooner or later. That seems a little odd, right? That doesn’t seem fair. So, you may be in exactly the same position in terms of the phase that you’re in, according to the National Academies or the CDC, but you may not get the vaccine at the same pace.”
The way vaccines are allocated across states also has ethical ramifications.
“How much each state gets from the federal government is an ethics question,” said Dr. Kahn. “That’s about allocation across all 50 states. And the way that that’s been done has been, I would say, not the most ethically appropriate. It’s been based on what the proportion of the population your state is over the entire denominator of the United States, but that doesn’t take account of the fact that some states like mine (Maryland) have a much higher proportion of healthcare workers than another state like North Dakota.”
Another important ethical concern is ensuring equitable distribution of vaccines to the demographics most affected by COVID-19.
“Ethnic minorities have been the hardest hit: Black and Latinx American Populations are nearly three times as likely to die of COVID as white Americans are,” explained Dr. Aiyar. “How can we ensure that these communities get the vaccine as quickly as possible?”
Dr. Montgomery Rice noted that she listened in on the Advisory Committee on Immunization Practices (ACIP) hearings (which informed the CDC guidelines) about vaccine distribution and was happy to hear that Tier 1 (the first group of people to be vaccinated including healthcare personnel and residents of long-term care facilities) recommendations will ensure that ethnic minorities are well-represented.
“They talked about justice and equity, and it really was threaded throughout the recommendations: they put on an equal standing physicians, nurses, and healthcare personnel,” she remarked. “So, anybody working in the healthcare system, anybody there who has a point of contact with the patient – whether you work in food services, as a radiology technician, or a front desk greeter – you have an equal right to get the vaccine…Across every one of those groups [in Tier 1], you’re going to have a very high number of underrepresented minorities, because they are often your frontline people.”
Logistics: How Do We Effectively Implement the Vaccination Guidelines?
The vaccine was developed in record time thanks to an all-hands effort by scientists worldwide, but now that the vaccines are being distributed by the states, there are a number of logistical hurdles to overcome.
“There was an incredible coming together of the research community [to develop COVID-19 treatments and vaccines],” remarked Ms. Solomon. “I think, however, there was so much focus on the accelerated development of these vaccines and treatments that we didn’t focus enough on the planning that needed to happen for these rollouts.”
At Morehouse School of Medicine, Dr. Montgomery Rice and her team have been planning vaccine ‘drive-throughs’ where people in Tier 1 can receive their vaccine, but scaling up these efforts across the nation is going to take more resources than institutions currently have, as well as some creative thinking.
“I spent the last two hours talking about logistics of how many people could we actually vaccinate from 9 AM – 4 PM on a Saturday while maintaining appropriate distance and all of the health preventive strategies,” she remarked. “Luckily for us, we see ourselves as a community stakeholder and we’re willing to do as much of this as we can with our costs. But we need true allocation of resources. This is not rocket science. If I order an iPhone or an Apple watch, I could have it in 48 hours. So, you telling me that we can’t figure out supply chain and logistics to get [vaccine rollout] done? Yes, we can, but it does require that we put resources in place.”
“We need to take every drive-through movie theater and make it a vaccination site,” she continued. “Things like that: that’s the level of creativity that we need, but that still takes resources because you’ve got to have the right circumstances where you can protect people in case someone has a reaction. It’s just a matter of having leadership and resources to get it done.”
Dr. Polsky stressed that while federal resources allocated earlier on could have helped accelerate vaccine distribution, we are still at the very beginning of the process and can expect improvements.
“We’re in month one. It’s like making that first pancake – it’s always the worst one. It takes a bit of time to get things heated up. Now, [the challenges] we’re going through in month one could have been avoided because we all saw it coming. But it’s not over. There’s a long road ahead. We need to get to the point where enough people get vaccinated, where there’s herd immunity.”
Hesitancy: How Can We Assure People are Comfortable and Willing to Get Vaccinated?
The panelists emphasized that fostering trust will be imperative for a successful vaccine rollout.
“The thing that we sorely need at the moment, maybe most of all, is trust in what’s happening now,” said Dr. Kahn. “We have to invest in whatever it takes to build trust at this moment, as we make our way through the final stages of this pandemic.”
Dr. Montgomery Rice highlighted the need for effective communication to those hesitant to receive the vaccine, and her focus is on fostering trust within the African-American community.
“The first thing that we had to take in consideration was the historical context of African-Americans and the health system,” she explained. “We’ve had to deal with all of the concerns that people have as it relates to African-Americans participating in research voluntarily or involuntarily… We’ve had multiple forums. And in fact, we have another town hall tonight. We will probably have 30,000 people online talking about this. And we will have some people who are in the Biden/Harris transition who are dealing with COVID-19. So, we’ve tried to create forums where people could ask any question that they wanted to ask. And we weren’t dismissive because we have to move from vaccine hesitancy to vaccine acceptance.”
Dr. Montgomery Rice stressed that certain terminology, such as the federal government’s ‘Operation Warp Speed’ program for COVID-19 vaccine development, can fuel hesitancy.
“‘Warp speed’ was not a good term. Warp speed is in Star Wars and Star Trek, but warp speed is not what you want to use for developing a drug or intervention that you want a mass number of people to use. We had to spend a lot of time letting people know that warp speed did not mean that we had skipped a step. In fact, there were no steps skipped, and we’ve had to communicate to people that there were Black and Brown people at every stage of development.”
Critically, Dr. Montgomery Rice also acknowledged a need for public visibility of minorities receiving the vaccine. She herself received the vaccine on CNN alongside Chief Medical Correspondent Dr. Sanjay Gupta.
“This is another thing that really does matter: we’ve shown pictures of people getting the vaccine. We hosted an event where we actually vaccinated about 30 of the civil rights leaders who are 75 and above: Ambassador Young, former HHS Louis Sullivan (who was the founder of Morehouse School of Medicine), Hank Aaron, and Hank Thomas (one of the freedom riders), to name a few. And we did that so that people would see that we wouldn’t put something in people’s arms, particularly people that we care about, if we didn’t think it was safe. And now, we have gotten 1,500 calls just between Monday and today of people ready to get their vaccine.”
Economics: What Resources Do We Need to Get This Done?
The panelists underscored the need for federal funding to equip states for vaccine rollout.
“We need to align planning and structure with resources – and that’s what we have not seen,” remarked Dr. Montgomery Rice. “It’s something we would hope to see from our leadership at the state and federal levels. Our state officials want to do the right thing – but they are exhausted from testing and contact tracing, and they haven’t been given the resources to support [the vaccine rollout].”
Although significant funding is required to distribute the vaccines, Dr. Polsky is certain the economic benefits will be worth it.
“Is there a return on investment to speeding this up? If we hit some threshold of immunity, the economy will start up, and things will get back to normal,” remarked Dr. Polsky. “The sooner we hit that number, things will start to flow in a different way. Take, for example, this $9 billion investment [in the distribution of vaccines]. If we had gotten that just a week earlier, or another billion dollars several weeks earlier, that would pay for itself in terms of how the economy rebounds. The way we are operating now, it’s like building this gorgeous castle, but never building the road to get there.”
Dr. Kahn agrees that we need to pour as many resources into vaccination as we can.
“What kind of costs have we incurred? Think about the education of our children: you can’t get back a year of school for some of these kids,” he said. “I’m with you, Dan. It seems to me that the price doesn’t matter. We sort of acted that way anyway for the last 10 months, so why all of a sudden are we starting to think about whether this is an appropriate return on an investment?”
Ms. Solomon noted that once the economy is back up and running like normal, there will likely be a boom of activity rather than recession-like behavior.
“One thing I find interesting is that experts say the economy is not going to act like a recession – it’s going to act like a national disaster,” she recalled. “Once we pull out of the national disaster, there’s just a tremendous amount of pent-up demand for all kinds of things. I mean, who wouldn’t want to go to the movies or go to a restaurant or, you know, just do anything?”
Getting Through the Pandemic Together
While the pandemic has made life extremely challenging, the panelists reflected on lessons learned and their optimism that the vaccines will lead to better days.
“Let’s just stay focused on the goal. And the goal is really to get people vaccinated and understand that we have very good guidelines and recommendations,” said Dr. Montgomery Rice. “We need to share those plans broadly so that we can execute more efficiently and more effectively.”
“Getting vaccinated is not always convenient or easy. It can be scary. Everyone has some fears, but I think it’s important not just for your own health, but for the health of everyone around you,” stressed Dr. Polsky.
“There really is a light at the end of the tunnel,” remarked Ms. Solomon. “We really are going to get back to something that’s pretty close to our normal. Maybe we’re going to be wearing masks for a while longer, but we are going to get there. Don’t give up hope.”
“Transparency is going to be really important as we continue through this. And just to reiterate what Susan said, we’re all in this together,” added Dr. Kahn. “Not everybody’s going to get [the vaccine] exactly when they want it. And I think we all have to remember that our turns will come. We’re all going to be better off if we handle this well and get vaccinated.”