Stem Cell Study Reveals How Neurons From PTSD Patients React to Stress
First induced pluripotent stem cell model of PTSD offers insights into underlying genetics and opportunities for new therapies (Sign...
What is PTSD?
Post-traumatic stress disorder (PTSD) is a mental health condition that’s triggered by a terrifying event or trauma — either experiencing it or witnessing it. PTSD is especially prevalent among military veterans. Symptoms may include flashbacks, nightmares and severe anxiety, as well as uncontrollable thoughts about the event. However, not all individuals who experience traumatic events develop PTSD, so a major question in PTSD research is why only some individuals develop these symptoms.
How is NYSCF Using Stem Cells To Study PTSD?
The goal of our PTSD research is to understand how genetics contributes to stress response in the brains of combat veterans. Understanding difference in stress response at the cellular level could explain why some individuals are more susceptible to PTSD than others.
At the NYSCF Research Institute, we are using our own, powerful robotic platform to create stem cells for research. Our NYSCF Global Stem Cell Array® can rapidly, efficiently, and reproducibly create stem cells from skin or blood, and then reprogram these cells to become the brain cells impacted by PTSD.
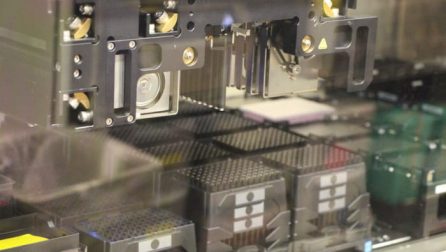
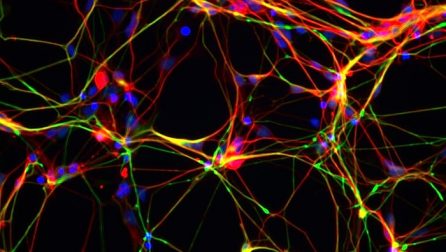
Our collaborators at the U.S. Department of Veterans Affairs and the Icahn School of Medicine at Mount Sinai have collected blood and skin biopsies from combat-exposed veterans with and without PTSD. We turned these skin cells into stem cells using the Array before converting them into different types of neurons. Next, we exposed these neurons to synthetic hormones that mimic stress, allowing us to observe how PTSD and non-PTSD patient brain cells respond, looking at whether there are identifiable features which distinguish how the cells of different people respond to stress. This work is allowing us to investigate new genetic risk factors for PTSD and potential preventative measures or treatments.
Carina Seah, Michael S. Breen, Tom Rusielewicz, Heather N. Bader, Changxin Xu, Christopher J. Hunter, Barry McCarthy, PJ Michael Deans, Mitali Chattopadhyay, Frank Desarnaud, Iouri Makotkine, Janine D. Flory, Linda M. Bierer, Migle Staniskyte, NYSCF Global Array Team, Scott A. Noggle, Laura M. Huckins, Daniel Paull, Kristen J. Brennand, Rachel Yehuda. Nature Neuroscience. 2022. DOI: https://www.nature.com/articles/s41593-022-01161-y
This study, a collaboration with the Icahn School of Medicine at Mount Sinai and the Office of Veterans Affairs, demonstrates that we can use stem cells to identify genetic and cellular hallmarks of PTSD risk. We have distinguished PTSD and non-PTSD patients by computational analysis, indicating that there are identifiable features which show how the cells of different soldiers respond to stress. It also indicates that these stress response features may correspond to whether or not a soldier will develop PTSD. We are following up on the preliminary data by more closely analyzing genes predicted to be risk factors for PTSD.
First induced pluripotent stem cell model of PTSD offers insights into underlying genetics and opportunities for new therapies (Sign...
The Context: Post-traumatic stress disorder (PTSD) affects more than 12 million people worldwide. Only a minority of people exposed...
Why do some people get PTSD and others don’t? And what can stem cells tell us about how to...
Studies suggest PTSD has a significant genetic component, but more research is needed to understand the genetic risks and how these lead to dysfunction in the brain. NYSCF is using stem cells from many different individuals to create the actual cells affected by PTSD and investigate the role of genetics in PTSD.
PTSD is typically brought on by a very stressful, frightening, or distressing event, or after a prolonged traumatic experience. Types of events that can lead to PTSD include serious accidents, combat, or physical or sexual assault, among others.
PTSD is thought to potentially affect the brain through hypersensitivity to stress, which was the driver of our latest study, but much is still left to learn about how exactly the disorder plays out in the brain. Stem cells give us a window into the brain to tease apart these causes on a cellular level, investigating how neurons respond to stressors.
About 6 out of every 100 people (or 6% of the population) will experience PTSD, and the disorder affects about 12 million adults in the United States each year. Women are also more than twice as likely to develop PTSD than men (10% for women and 4% for men).
There is currently no cure for PTSD, but there are several treatments that help manage symptoms, including cognitive behavioral therapy and several approved medications.
What is Schizophrenia?
Schizophrenia is a serious mental disorder in which people interpret reality abnormally. Schizophrenia may result in some combination of hallucinations, delusions, and extremely disordered thinking and behavior that impairs daily functioning, and can be disabling. We know there is a genetic component to schizophrenia, and understanding this relationship will be key for developing much-needed treatments.
How is NYSCF Studying Schizophrenia with Stem Cells?
The goal of our schizophrenia research is to discover how gene expression (how different genes are turned on or off) differs in the brains of individuals with and without schizophrenia. This is poorly understood because of the difficulty in studying gene expression in the brain: it can traditionally only be done by collecting tissue from the brains of deceased patients.
With stem cells, however, we can create the brain cells affected by schizophrenia from the skin or blood of a patient. At the NYSCF Research Institute, we are using our own, powerful robotic system to create stem cells for research. Our NYSCF Global Stem Cell Array® can rapidly, efficiently, and reproducibly create stem cells, and then turn these cells into the brain cells impacted by schizophrenia.
Our collaborators at the Icahn School of Medicine at Mount Sinai have collected skin samples from schizophrenia-affected patients and non-affected people. Our scientists then turn these into stem cells using the Array, and then into the brain cells affected by schizophrenia, allowing us to study how these cells turn certain genes on or off in patients.
Oligodendrocyte differentiation of induced pluripotent stem cells derived from subjects with schizophrenias implicate abnormalities in development
Donna L. McPhie, Ralda Nehme, Caitlin Ravichandran, Suzann M. Babb, Sulagna Dia Ghosh, Alexandra Staskus, Amy Kalinowski, Rupinderjit Kaur, Panagiotis Douvaras, Fei Du, Dost Ongur, Valentina Fossati, Kevin Eggan & Bruce M. Cohen. 2018. Translational Psychiatry. DOI: https://doi.org/10.1038/s41398-018-0284-6
In this study, a team including NYSCF scientists found that patients with schizophrenia tended to produce fewer oligodendrocytes than those without the disorder, potentially leading to issues with connectivity and signaling within the brain.
What they did: A team of scientists including NYSCF Scientific Advisor and Harvard University Professor of Stem Cell and...
The Context: 1 in 3,000 people has a genetic defect called 22q11.2 deletion syndrome, or 22q11DS, putting them at...
The Context: Studying brain development can be difficult since scientists cannot easily access developing brain tissue. Creating models of...
Schizophrenia is known to have a genetic component, but much is left to learn about how genetics impact one’s risk for developing the disorder. Risk is not tied to a single gene, but is rather likely the result of several genetic variants. NYSCF is using stem cells to tease apart the genetic drivers of the disease.
Positive symptoms of schizophrenia refer to changes in behavior or thoughts including hallucinations, delusions, and disorganized thinking.
Negative symptoms of schizophrenia refer to withdrawal from typical behavior and/or the world around them. Such symptoms include loss of motivation, interest, social skills, and sleep.
Schizophrenia is thought to be related to chemical imbalances in the brain as well as structural and functional differences. It can be hard to study a schizophrenia-affected brain before a patient has passed away, but stem cells give us a unique window into the brain by allowing scientists to create the actual cells affected by the disease.
According to the World Health Organization, schizophrenia affects about 24 million people worldwide.
Schizophrenia symptoms typically do not appear until one’s mid-to-late 20s or as late as one’s 30s.