Hidden Signatures of Parkinson’s Disease Revealed by NYSCF’s Automation Technology and Artificial Intelligence
NewsThe Context: The vast majority of drugs fail clinical trials, largely because there is still much we do not understand about the underpinnings of complex diseases like Parkinson’s or Alzheimer’s, and most drugs are discovered using animal models that do not adequately capture how a disease manifests in humans. We need a better system for discovering exactly how our cells react to disease so that we can figure out how to treat them.
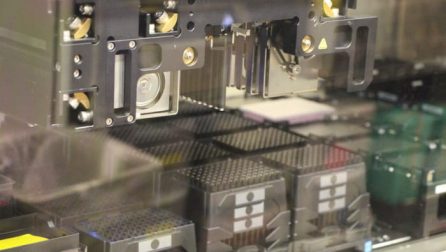
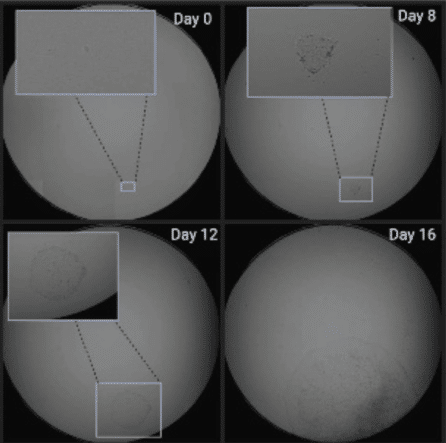
The Study: A new platform developed by NYSCF scientists integrates robotic systems for studying patient cells with artificial intelligence methods for image analysis to identify cellular features of disease. Their collaborative study with Google Research, published today in Nature Communications, examined more than 6 million images to successfully identify new hallmarks of Parkinson’s patient skin cells in comparison to healthy controls.
The Importance: This platform allows scientists to study diseases like Parkinson’s at an unprecedented cellular level, identifying features of disease invisible to the human eye that can be targeted by new or existing drugs. The system could also distinguish subgroups of Parkinson’s patients with varying features, which is key groundwork for advancing personalized medicine.
Typical drug discovery starts with a mouse. Scientists simulate a disease like Alzheimer’s or Parkinson’s in the mouse and see if they can pinpoint any aberrant features to target with drugs. If a drug works in the mouse, it is taken to clinical trials. Then, in the vast majority of cases, it fails. Why?
“Part of why so many drugs fail is because drug developers have had to rely on mouse models whose biology is just completely different from human patients, as well as preconceived notions about what is driving the disease, which typically have ended up being wrong or do not hold true for every patient,” explained NYSCF CEO Susan L. Solomon, JD.
But a mouse isn’t a human. We need to study human diseases in human cells to find drugs that will work in human patients. And beyond this, we need to leverage new technologies for examining these cells in extraordinary detail, because drivers of disease are often hard to spot, and can vary from person to person.
“We have built robotic technology that allows us to study human cells from the patients themselves from large populations that generate vast amounts of human data,” explained Ms. Solomon. “This allows us to more accurately study features of PD at the level of cells and discover treatments that actually work across different patients or even groups of patients.”
Artificial Intelligence Uncovers the Intricacies of PD
What if the features of disease are so small – so intricate – that we can’t detect them with the human eye? This is where artificial intelligence comes in.
Essentially, the platform works a bit like the technology that recognizes your face to unlock your phone. An algorithm studies lots of images of cells (in this case, 6 million, accounting for 48TB of data), and learns how to distinguish between those from healthy individuals and those with PD. The more images it studies, the better it gets.

“Our platform was able to tell the difference between healthy cells and cells from Parkinson’s patients,” explained Daniel Paull, PhD, SVP of Discovery and Platform Development. “It could even pinpoint the exact donor that a given sample came from. In Parkinson’s research, we often lack the tools to tease apart these minute differences, but here we were able to do just that.”
“These artificial intelligence methods can determine what patient cells have in common that might not be otherwise observable,” said Samuel J. Yang, Research Scientist at Google Research. “What’s also important is that the algorithms are unbiased — they do not rely on any prior knowledge or preconceptions about Parkinson’s disease, so we can discover entirely new signatures of disease.”
Phillip Nelson, Director of Engineering at Google Research, also noted that this is an exciting collaboration because for AI to reach its full potential, it needs large amounts of standardized data to ensure its underlying algorithm is trained correctly and is producing accurate results. This kind of scale is only achievable through NYSCF’s robotic systems.
“NYSCF is especially eager to do the heavy lifting that makes for good science: to introduce automation and minimize variance,” he said. “It’s something that people talk about a lot, but NYSCF actually does it. We’ve done tremendous work together and we’re looking forward to doing a lot more work together in the future.”
“This is an ideal demonstration of the power of artificial intelligence for disease research,” added Marc Berndl, Software Engineer at Google Research. “We have had a very productive collaboration with NYSCF, especially because their advanced robotic systems create reproducible data that can yield reliable insights.”
The researchers credit a ‘team science’ approach to the success of the study.
“This study was a massive collaboration between many teams: the disease researchers, data scientists (such as myself), and engineers at NYSCF along with computer scientists and engineers at Google,” noted Bianca Migliori, PhD, Senior Staff Data Scientist at NYSCF. “It was really exciting to see what is possible when such talented people combine forces.”
What’s Next?
“We now hope that we can leverage this platform to discover better Parkinson’s drugs,” said Dr. Paull. “We’ve begun screening tens, to hundreds, to thousands of drugs in order to reverse the disease signatures that we are detecting and make sick cells healthy again.”
PD is just the beginning – the team is now applying the platform to other diseases for which current treatments are lacking, introducing an entirely new paradigm for finding drugs that actually work on human cells.
“We hope to be able to take this beyond Parkinson’s disease,” said Dr. Paull. “We’re already investigating a number of other diseases to see if we can similarly detect this disease signature in those cells.”
“We’ve needed a new model for a long time,” added Ms. Solomon. “The combination of [NYSCF’s technology] with very powerful artificial intelligence, in my opinion, is a home run.”
Read the press release here.
Cover image: Skin cells generated by the Array and used to study PD
Journal article:
Integrating deep learning and unbiased automated high-content screening to identify complex disease signatures in human fibroblasts
Lauren Schiff, Bianca Migliori, Ye Chen Deidre Carter, Caitlyn Bonilla, Jenna Hall, Minjie Fan, Edmund Tam, Sara Ahadi, Brodie Fischbacher, Anton Geraschenko, Christopher J. Hunter, Subhashini Venugopalan, Sean DesMarteau, Arunachalam Narayanaswamy, Selwyn Jacob, Zan Armstrong, Peter Ferrarotto, Brian Williams, Geoff Buckley-Herd, Jon Hazard, Jordan Goldberg, Marc Coram, Reid Otto, Edward A. Baltz, Laura Andres-Martin, Orion Pritchard, Alyssa Duren-Lubanski, Ameya Daigavane, Kathryn Reggio, NYSCF Global Stem Cell Array Team*, Phillip C. Nelson, Michael Frumkin, Susan L. Solomon, Lauren Bauer, Raeka S. Aiyar, Elizabeth Schwarzbach, Scott A. Noggle, Frederick J. Monsma Jr., Daniel Paull, Marc Berndl, Samuel J. Yang, Bjarki Johannesson. Nature Communications. 2022. DOI: https://doi.org/10.1038/s41467-022-28423-4
Read additional press coverage in:

