Progress, Challenges, and Promise: On the Road to a Type 1 Diabetes Cure
News Video“How many people were promised a cure [for type 1 diabetes] within five or ten years?” JDRF CEO Aaron Kowalski asks the audience. Half the hands go up.
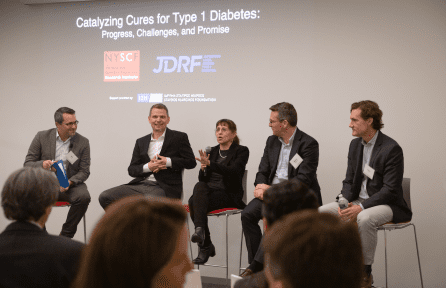
For 98 years, we have used insulin therapy to treat the symptoms of type 1 diabetes (T1D), but there is still no cure for the disease. At a recent panel discussion held at the NYSCF Research Institute, scientists, clinicians, and patient advocates discussed the latest progress towards cures for T1D, including NYSCF’s work to develop a cell replacement therapy.
The discussion was moderated by Ben Goldberger (executive editor, TIME), and featured Jason Baker, MD (Assistant Professor of Medicine, Weill Cornell Medical Center), Bjarki Johannesson, PhD (Senior Research Investigator, The NYSCF Research Institute), Aaron Kowalski, PhD (President and CEO, JDRF), and Carol Levy, MD (Director, Mount Sinai Diabetes Center).

“I’ve been a diabetic for a couple of decades now,” said Mr. Goldberger, who has this in common with Drs. Baker, Kowalski, and Levy. He expressed his excitement to hear from researchers doing pioneering work, many of whom have experienced the toll of T1D themselves.
“This group has a remarkable range of experience, interests, backgrounds, and distinct specialties,” he remarked.
Current Treatments
In T1D, the immune system makes a mistake: it attacks healthy, insulin-producing pancreatic beta cells. Because of this, T1D patients must administer their own insulin, often through injections. If you’re a T1D patient, keeping track of your own blood sugar levels, closely monitoring your diet, determining how much insulin to inject, and then performing the procedure yourself is a lot to manage.
Luckily, the new technologies are making the treatment process easier. For example, constant glucose monitoring (in which a sensor is placed under the skin and checks a patient’s blood sugar levels every five minutes) has been a game changer for many patients. Integration of this technology into a system called a ‘closed loop’ or an ‘artificial pancreas’ can be even better—taking injections out of the equation altogether.
“You’ve got an insulin pump, a glucose sensor, and an algorithm. Data from the sensor goes to the pump, and the algorithm tells the pump how much insulin to deliver,’ explained Dr. Levy, whose work focuses on optimizing this system. “Many people with diabetes are quite good at taking care of their blood sugar, but they’re not perfect. Nobody is perfect. So that’s where machine learning can really take over and relieve some of the burden.”
Dr. Baker stressed that while new technologies show a lot of benefits, every patient is different, and these treatments aren’t necessarily one-size-fits-all.
“I’m a definite lover of technology, but I don’t think that a technological advancement is really going to fit everybody,” he added. “It’s a beautiful thing for people to be able to pick and choose which system they would like. I think we’ve come a long way with the technology, but there’s still a long way to go.”
Toward Cures
While there are many exciting technologies aiding in T1D management, the ultimate goal is to reach cures. NYSCF is on a mission to get there with stem cells, an effort that Dr. Johannesson is leading.
“What we do in the lab is take patient skin cells or blood cells, and we use our advanced robotic system to create stem cells,” he explained. “You change those into pancreatic beta cells and then you transplant them back into the patient.”

It sounds simple enough, but since T1D is an autoimmune disease, the immune system will still attack the new cells. How can researchers disguise the beta cells from the rogue immune system?
“The idea we came up with was to use genome editing, which allows you to go into the cells’ DNA and modify it in very precise ways,” Dr. Johannesson described. “So, you can take out genes, you can add genes, you can control which genes are being expressed — it’s really a phenomenally powerful technology. And the idea here was to modify the stem cells in a way that they would become less visible to the immune system.”
This way, when the modified stem cells are turned into beta cells and transplanted into a patient, they would essentially be camouflaged from the immune system.
Cell therapies have been employed to treat T1D before — some patients have received islet transplantations of groups of pancreatic cells from a deceased organ donor. But as Dr. Kowalski noted, this therapy is limited by the number of organ donors available.
“There have been about 5,000 islet transplants, all in the last 20 or so years. There are 30 – 40,000 new T1D diagnoses in the U.S. every year. So, you have a huge supply and demand issue. You need to take what’s going on in the lab and then scale it up. You have to make it applicable to everybody. That’s why the capabilities here [at NYSCF] are so stunning.”

Dr. Kowalski also expressed that cures can come in different forms, and there is a lot to look forward to in the future.
“The story here [at NYSCF] of the pioneering work that’s happening — that this team has catalyzed — shows that there’s no singular approach, but that the promise of the work is very, very real.”
Check out highlights from the panel:

