When Good Brain Cells Go Bad: New Findings from NYSCF and Johns Hopkins Precision Medicine Initiative
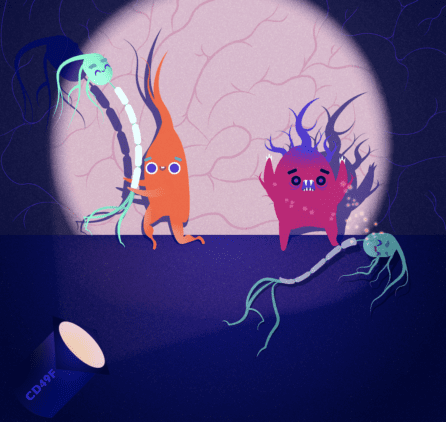
NewsThe Context: Astrocytes are support cells in the brain that help our neurons function properly. However, these typically helpful cells can ‘go rogue’ or ‘reactive’ in the presence of brain inflammation – a common hallmark of neurodegenerative diseases like Alzheimer’s or multiple sclerosis (MS) – making them harmful to the cells they typically support.
The Study: Two new studies published in Frontiers in Molecular Neuroscience by NYSCF’s Valentina Fossati, PhD, explore how reactive astrocytes contribute to diseases like Alzheimer’s and MS. The first study, led by Dr. Fossati, provides the most in-depth characterization of these cells to date, and finds evidence of them in the brains of deceased Alzheimer’s patients. The second study, led by Peter Calabresi, MD, at Johns Hopkins, as part of NYSCF’s precision medicine partnership with Johns Hopkins University School of Medicine and Bloomberg Philanthropies, discovers that reactive astrocytes may contribute to MS by inhibiting cells that create myelin – an important substance that insulates neurons so they can transmit electrical signals.
The Importance: These studies represent crucial groundwork toward understanding the role of reactive astrocytes in neurodegenerative diseases, and open the door for development of more effective therapies.
Inflammation is a natural response that our body launches to combat external insults such as viral infections or wounds. It involves the activation of an army of immune cells and the release of chemical signals that help us get rid of the intruders. However, even though it protects us in many circumstances, inflammation can also be a symptom of many chronic diseases.
“Inflammation is present in many diseases such as Alzheimer’s disease, multiple sclerosis, and even COVID-19,” noted Dr. Fossati. “Inflammatory signals can ultimately lead to cellular damage and fuel the process of neurodegeneration.”
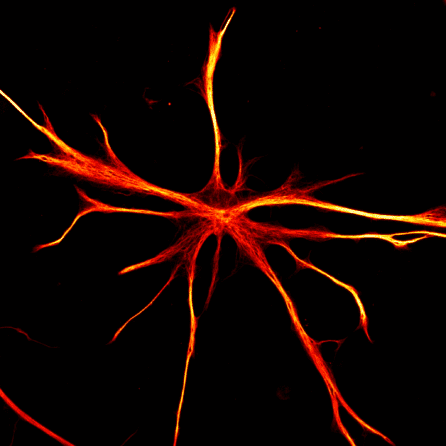
In brain diseases, it is not only the immune cells in the blood that can cause harm, but also other cell types already present in the brain, such as astrocytes. Astrocytes – named for their ‘star-like’ structure – are the most abundant cell population in the brain, and typically provide vital aid to neurons. But in the presence of inflammation, these cells can ‘go rogue’ and become toxic to the cells they normally support.
“We have more and more evidence suggesting that astrocytes play a critical role in disease,” remarked Dr. Fossati. “They take on a destructive state – what we call ‘reactive astrocytes’ – and can become toxic, directly killing neurons”.
Dr. Fossati, continuing a longstanding collaboration with Dr. Shane Liddelow, sought out to investigate the implications that reactive astrocytes have for neurodegenerative diseases in two new studies, published this week in Frontiers in Molecular Neuroscience.
Separating Harmful Astrocytes From Helpful Ones
To understand their errant behavior in disease, researchers first needed to understand what sets reactive astrocytes apart from normal astrocytes and other brain cells.
The team created astrocytes from stem cells using a special method developed by Dr. Fossati’s team, and then exposed the astrocytes to an inflammatory environment – mimicking that found in the body of a patient experiencing neurodegeneration.
The astrocytes then became reactive, and in collaboration with Dr. Junmin Peng‘s lab, the team looked at the proteins being produced by the cells to compare the rogue astrocytes to their healthy neighbors. Measuring these proteins helps the scientists identify the critical roles of reactive astrocytes in inflammation and the immune response.
“We had previously looked at what genes are activated in reactive astrocytes, but here we wanted to find out what proteins they make [that make them different from healthy astrocytes], and what signals they are sending around to neurons and to other cells,” noted Dr. Fossati.
Importantly, the team identified six proteins uniquely present on the surface of reactive astrocytes, which can now be used to separate them from normal astrocytes and study them up close, setting the stage for future studies and treatment development
“We found that these proteins were highly expressed in brain samples from Alzheimer’s patients, and we want to continue exploring their potential presence in MS, Parkinson’s, and all other neurodegenerative diseases.”
Rogue Astrocytes Interfere with the Brain’s Signaling System in MS
In the second study, the scientists, led by Dr. Calabresi looked at how reactive astrocytes in multiple sclerosis patients may interfere with the brain’s ability to send signals.
“The hallmark of MS is something called ‘demyelination,’” explained Dr. Fossati. “We have cells in our brains called oligodendrocytes that create a substance called myelin that coats our neurons and helps them talk to each other.”
“In MS, these oligodendrocytes are attacked by immune cells, impairing their ability to myelinate neurons. Therefore, there is a huge push to find therapies that restore myelination. However, we have to make sure that in those therapies, we protect oligodendrocytes from being damaged, and we suspect that reactive astrocytes could be contributing to the degradation of these cells along with the immune cells.”
The team set out to explore how reactive astrocytes may affect oligodendrocyte function by comparing astrocytes made from the stem cells of people with MS to those made from healthy controls – taking a closer look at how the astrocytes’ behavior in inflammatory environments impacts oligodendrocytes.
“We found that astrocytes in inflammatory environments are releasing signals that interfere with the process of remyelination,” reported Dr. Fossati.
Specifically, reactive astrocytes appear to impair an oligodendrocyte’s ability to mature, in turn preventing it from making myelin. The team stresses that understanding this process will be critical for developing remyelination treatments.
“I think that is going to be hugely important for all neurodegenerative diseases,” said Dr. Calabresi in a virtual panel discussing inflammation in neurodegeneration. “It makes perfect sense to me that the astrocytes and the other glial cells are mediating this toxicity.”
“This is really important groundwork as we continue to develop new therapies for MS,” remarked Dr. Fossati. “We look forward to continuing our work with Dr. Calabresi and the teams at NYSCF and JHU to further investigate the role of reactive astrocytes in MS and many other neurodegenerative diseases.
Journal articles:
Proteomic alterations and novel markers of neurotoxic reactive astrocytes in human iPSC models
David Labib, Zhen Wang, Priya Prakash, Matt Zimmer, Matthew D. Smith, Paul W. Frazel, Lilianne Barbar, Maria L. Sapar, Peter A. Calabresi, Junmin Peng, Shane A. Liddelow, and Valentina Fossati. Frontiers in Molecular Neuroscience. 2022. DOI: https://doi.org/10.3389/fnmol.2022.870085
Reactive astrocytes derived from human induced pluripotent stem cells suppress oligodendrocyte precursor cell differentiation
Matthew D. Smith, Xitiz Chamling, Alexander J. Gill, Hector Martinez, Weifeng Li, Kathryn C. Fitzgerald, Elias S. Sotirchos, Marjan Gharagozloo, Pavan Bhargava, Donald J. Zack, Valentina Fossati and Peter A. Calabresi. Frontiers in Molecular Neuroscience. 2022.

