Human Brain Cells Take Up Residence In Rat Brains to Illuminate the Secrets of Neuropsychiatric Disease
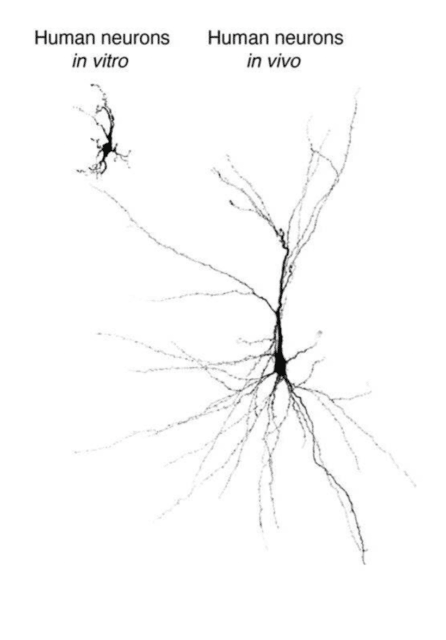
NewsThe Context: Neuropsychiatric disorders are notoriously hard to study due to their complexity and the inaccessibility of human brain tissue for experimentation. However, recent advances in stem cell technology such as ‘organoids’ – 3D clusters of human brain tissue made from stem cells – are helping researchers better understand how human brain cells interact, develop, and dysfunction. Organoids bear certain limitations because they cannot fully mature and function the way they would in a living organism, however, and cannot receive sensory information from their surrounding environment.
The Study: Scientists have created brain organoids and transplanted them into rats to study the developing brain in unprecedented detail. The transplanted cells were able to react to sensory information from the rats’ environments, and were also successful at capturing the biology of a neuropsychiatric condition called Timothy Syndrome, suggesting this approach could be used to tease apart the underpinnings of disease. The study, led by NYSCF – Robertson Stem Cell Investigator Sergiu Pasca, MD, of Stanford University, appears in Nature.
The Importance: This new model can be used to study conditions like autism spectrum disorder, ADHD, and schizophrenia in more depth than ever before, and could also serve as a platform for drug testing and therapeutic development.
“We can now study healthy brain development as well as brain disorders understood to take root in development in unprecedented detail, without needing to excise tissue from a human brain,” said Dr. Pasca, the Bonnie Uytengsu and Family Director of Stanford Brain Organogenesis, in a press release. “We can also use this new platform to test new drugs and gene therapies for neuropsychiatric disorders.”
Connecting a Brain with the World Around It
A key for studying neuropsychiatric diseases that previous studies have missed is the integration of sensory information from one’s surrounding environment – a critical factor for a developing brain.
“It’s the stuff that we get after we are born,” Paola Arlotta, PhD, NYSCF Scientific Advisor and a prominent brain organoid researcher at Harvard University who was not involved in the study told NPR. “Especially when we begin to experience the world and hear sound, see light, and so on.”
“We’ve been making ever more complicated circuits in a dish using organoids and sophisticated combinations of them, called assembloids,” said Dr. Pasca. “But neurons within these lab dishes are still lagging behind in their development compared with what you’d see in a naturally developing human brain.”
Human Cells Take to a Rat Brain
The team wondered if they could make a more complete model of a developing brain by transplanting their human organoids into living creatures – in this case, two-day-old rat pups. These still-developing pups would hopefully integrate the human cells into their brain circuitry (a much harder task for an adult brain).
Excitingly, the cells did just this. Rat cells penetrated the human brain implants and assembled into blood vessels, and rat immune cells in the brain also populated the human graft.
“They moved right in,” Pasca remarked.
And the implants didn’t just survive: they thrived.
“We discovered that the [organoid] grows, over the span of a few months, about nine times in volume,” Dr. Pasca told NPR. “In the end it covers roughly about a third of a rat’s hemisphere.”
Exploring Sensation & Reward in Transplanted Cells
The team then wondered, would these newly-integrated cells respond to external stimuli the way a typical brain would?
The scientists had placed the organoids in the rats’ sensory processing center, which picks up information from their whiskers about the world around them. To test whether the implants were receiving this information, they sent puffs of air to the rats’ whiskers, and watched the transplanted cells.
“When you stimulate the whiskers of the rat, the majority of human neurons are engaged in an electrical activity that follows that stimulation,” noted Dr. Pasca.
The team then conducted another experiment to test whether the implants had successfully infiltrated the rats’ reward centers. They started pairing a certain cue (in this case, blue light delivered to just the implanted cells) with a reward (water). Eventually, the rats began to associate the blue light with water – rushing to their spouts when the cue went on. This proved that the implants could successfully engage in reward learning – another unique brain characteristic that ties in with behavior.
Recapitulating A Neuropsychiatric Disorder
Finally, the team examined whether they could implant cells from a patient with Timothy Syndrome, a rare genetic disorder that affects brain development in ways that can cause symptoms of autism spectrum disorder, to model the disease.
“We’ve learned a lot about Timothy syndrome by studying organoids kept in a dish,” Dr. Pasca said. “But only with transplantation were we able to see these neuronal-activity-related differences.”
The researchers made organoids from Timothy syndrome patients and healthy controls. Once transplanted into the rat brains, they noticed the Timothy Syndrome cells were smaller and involved in very different electrical activity from the healthy brain cells.
“Once we transplanted and we looked 250 days later, we discovered that while control cells grew dramatically, patient cells failed to do so,” Dr. Pasca noted.
This suggests that Dr. Pasca’s model could be beneficial for uncovering features of disease that aren’t detectable in a dish.
What’s Next?
“It’s definitely a step forward,”remarked Dr. Arlotta. “The ultimate goal of this work is to begin to understand features of complex diseases like schizophrenia, autism spectrum disorder, bipolar disorder.”
That’s what Dr. Pasca will focus on next: applying his platform to different neuropsychiatric disorders.
“This is the most advanced human brain circuitry ever built from human skin cells and a demonstration that implanted human neurons can influence an animal’s behavior,” he said. “Our platform provides, for the first time, behavioral readouts for human cells and could, we hope, accelerate our understanding of complex psychiatric conditions.”
Cover image: Credit: Pasca Lab, Stanford University
Read more in: