Experts Unpack the First Stem Cell Model Study of PTSD and What it Means for Better Treatments
News VideoWhy do some people get PTSD and others don’t? And what can stem cells tell us about how to develop better therapies?
Understanding why certain individuals are susceptible to PTSD (and how to prevent or reverse it) has been a challenge, as scientists lacked the means to capture how the brains of prone individuals are affected by stress. A new collaborative study including NYSCF scientists reveals unique features of the PTSD brain by creating the first-ever stem cell model of the disorder from a cohort of 39 combat veterans exposed to trauma, half with PTSD and half without.
We recently gathered experts Rachel Yehuda, PhD (Icahn School of Medicine at Mount Sinai and Office of Veterans Affairs), Kristen Brennand, PhD (Yale University, NYSCF – Robertson Stem Cell Investigator Alumna), and Daniel Paull, PhD (The NYSCF Research Institute) to talk about their latest study that created the first-ever stem cell model of PTSD, and discovers new features of the disease that could be targeted therapeutically. The discussion was moderated by NYSCF’s Vice President of Scientific Outreach, Raeka Aiyar, PhD.
What is PTSD?
“PTSD is a psychiatric condition in which a set of symptoms or phenomena occur to people after they’ve been exposed to extreme trauma,” explained Dr. Yehuda. “It’s kind of like being haunted by the traumatic memory of something that happened to you. Some of the symptoms of PTSD revolve around having intrusive, distressing recollections of the event, having nightmares about it, and being very avoidant and hypervigilant. It’s a stress reaction that would be perfectly expected in the immediate aftermath of an event, but it just doesn’t seem to go away.”
How did this study come to be?
“We had an observation in the late 1980s that people with PTSD had lower cortisol levels [the body’s main stress response hormone] than people that didn’t have PTSD,” noted Dr. Yehuda. “And at the time, this was kind of an inconvenient truth because ‘stress theory’ basically said that with time, all the biological responses that you mobilize in response to stress can recalibrate. So the idea of finding low cortisol was almost a negation of the idea that people really continue to be marked by a traumatic experience and feel transformed by it.”
“That started us out on a very long path to try to understand what really happens in people that develop PTSD, and it became known to us very early on that only some people who are exposed to trauma develop PTSD.”
One important determinant of whether one develops PTSD is their genetics.
“In general, psychiatric disorders are highly heritable,” explained Dr. Brennand. “At the high end we have schizophrenia, where twin studies estimate the heritability to be over 80%. So that means, while yes, there’s an environmental component, 80% of your risk for schizophrenia is risk that you’re born with. Likewise, autism spectrum disorder, ADHD, and bipolar disorder are all also over 75% heritable. The other end of the spectrum, we have PTSD and depression, where twin studies estimate the heritability to be more like 30 to 35%.”

When Dr. Yehuda learned more about stem cells from Dr. Brennand, she thought they could be a perfect tool to model PTSD and evaluate how cells respond to stress.
“When I first met Dr. Brennand, and she told me about the ability to use this kind of technology to take cells back to their embryonic stage, I thought “wow, talk about doing a ‘before’ study!” she laughed. “It would be amazing to see what the neuronal or genetic architecture of these cells might be like from early on.”
“So then it became a question of, how do we undertake the most ambitious project I’ve ever dared to dream about? It was audaciously bold, and that’s when NYSCF came in. I approached Dan and said ‘I know you’ve been developing these robots. I’ve got a really clever experiment that will require all of them, and an amazing cohort that already exists thanks to Rachel’s efforts.’”
Why was NYSCF’s automation so useful for modeling PTSD?
When Dr. Brennand approached Dr. Paull, he knew this was exactly the type of experiment his team’s robots were primed to carry out.
“NYSCF has always been a champion of high risk experiments. For us personally, one of our big ones was building these automation tools and robotics to perform experiments with a level of reproducibility and control that is very hard to do by hand,” he said. “And then on top of that, be able to analyze lots of different people at the same time, because for many different diseases, the way to uncover whether there is something wrong inside the cells is to study as many as possible.”
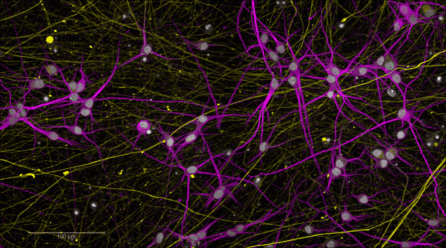
“We started bringing these robots into the lab with a very sort of ambitious goal of being able to make stem cells from lots of people in parallel. We were able to get that up and running, and so that led us to be an ideal collaborator in this study because not only could we help make the stem cell lines, but we could then also use the robots to turn these into neurons and do all the rest of the measures required by this study.”
“Thanks to Rachel and her team, we were able to collect samples from veterans who had served overseas, half with PTSD and half without,” he continued.
“We took blood samples and skin biopsies from these individuals and put those into our robots so that we could start turning them into stem cells. We then took those stem cells and turned them into brain cells that we analyzed.”
Why is it important to study the brains of PTSD patients?
“Before we embarked on this study, our lab had been working very intensively trying to develop a blood test to diagnose PTSD,” said Dr. Yehuda. “One of the things that we learned after more than a decade of studies is that when you take a blood sample from people with and without PTSD, there aren’t all that many differences between them. It’s not like a pregnancy test or a COVID test where you see a really clear result – rather there were teeny little signals that would come and go.”
“What happens in the blood is not necessarily what happens in the brain,” she continued. “And one of the most important findings that we had in this study is that the overlap between the genes that are expressed in blood and brain in response to stress hormones is pretty small. They have some in common, but they also have very different things that are activated because the blood and brain are different.”
What did the study find?
“Trauma exposure is a required element of a PTSD,” said Dr. Brennand. “You could have the highest risk in the world for PTSD, but if you live a charmed life and you’re never exposed to trauma, there would be no clinical impact of that risk.”
“That’s where we got the idea to incubate the neurons with stress hormones: hydrocortisone to be exact,” added Dr. Yehuda. “We decided that we might have a PTSD simulation in the dish, and we could then perhaps find a unique gene expression signature that could distinguish people with and without PTSD.”
“We tried delivering the stress hormones to the cells at different levels: some more mild, some highly elevated. Across all cells, PTSD and control, there was an enormous change overall once these neurons were exposed to the stress hormone,” noted Dr. Paull.
“But where the study obviously became of critical interest and real importance was that as we looked at the gene expression pattern, there was an incredible ability for us to distinguish cells that came from PTSD patients from those that came from healthy controls.”
The experiment also suggested that the experience of trauma in childhood could potentially affect brain circuitry.
“Another key part of this study was finding that it seems if you give a neuron a stressor very, very early on in its life, it might inhibit the way neurons grow and whether they form connections together,” said Dr. Paull.
“I think that almost everyone agrees now that earlier developmental trauma can have really intransigent, long lasting effects on the way that neuronal networks develop, and therefore dictates how people will respond to stress in the future,” added Dr. Yehuda. “It’s very important because when I went to graduate school, the prevailing model was that people can ‘get over’ earlier assaults because of the brain’s plasticity. But really the brain’s plasticity allows you to incorporate the environment even more. That doesn’t mean that you’re doomed [if you undergo early-in-life trauma], but it does mean that you’re changed. Environmental exposures change us, and that is really one of the important things that we demonstrate.”
What will this study mean for treatments?
The panelists are excited about the possibility of using their model for drug testing.
“There’s a large number of [drug] candidates to go after based on genetics and based on things that we’ve learned from previous work,” added Dr. Paull. “So in addition to giving a neuron a stimulant like hydrocortisone, what if you did that and then followed it up with a drug of some sort? Would that dampen the response? Would that make the PTSD-affected cells look more like the healthy controls?”
“Now we are starting to do research with psychedelic drugs, and we’re drawing from this cohort of patients so that we have an opportunity to use the findings that we have collected to see whether we can predict responses to certain medications,” said Dr. Yehuda.
“We are even able to take these same cells that we have generated and test how they respond to any number of drugs. We might be able to, in the future, have a very elegant way of being able to identify – before we start to do a whole lot of different treatment approaches – who might be best suited for what kind of treatment,” she continued.
“And that’s really why all of us got so excited about doing this study, because it was ambitious. But it’s really important for the public to have hope that in the near future, we will be able to use these kinds of scientific advances in the service of their healthcare, and the service of being able to have better strategies for deciding how we treat patients.”
What future directions will this research take?
Women are more than twice as likely to develop PTSD than men, and the disorder is more prevalent in minorities as well. The researchers plan to further explore whether there are any biological factors that underlie these disparities.
“This first study was done with cells from all men, and Rachel’s been determined to add women,” noted Dr. Brennand. “We would also like to do sub-analyses or secondary analyses to see whether there are racial differences in the response. So this is where these kinds of questions become very important. This model is a nice way to be able to examine things from early time points.”
The scientists will also begin to explore stress responses in other types of brain cells.
“We started with one major cell type in the brain: glutamatergic neurons, but we don’t think that’s the only one implicated in PTSD. And so we’ve already expanded this to a second cell type, GABAergic neurons, and I don’t think we’re going to stop there,” said Dr. Brennand. “I think what’s really gonna be important is mixtures of the cell types implicated in PTSD and understanding the way these cell types act both alone and in circuits, and really getting to higher level links between the genetics and the activity differences that are happening in response to stress.”
What is most exciting to the scientists about this research?
“I think it’s two things,” remarked Dr. Paull. “First is our automated platform, which is ‘disease agnostic’ in a way. We can take cell types that are specific to a given disease and investigate them in much the same way we have here. I think that’s one whole area that’s just getting very, very exciting.”
“I think specifically coming out of this study, we don’t necessarily understand what some of these new therapies actually do in these cells,” he continued. “And so yes, we used cortisol here because we wanted to invoke a response, but in much the same way, if we were to take any drug and put it onto these cells, maybe we can actually begin to understand mechanistically what is happening inside these cells in response to those drugs.”
Dr. Brennand is also interested in using stem cells as a model to advance personalized medicine.
“The idea that I find most intriguing is as we better understand the risk, and this is true across brain disorders, we’re finding that there’s points of convergence in individual risk genes across people, and this moves us towards bucketing patients,” she said.
“If we can begin to figure out that there are multiple subsets of PTSD who respond to drugs differently – if the genetics can tell us that people who show certain similar cellular features respond best to this drug – we could use that as an informed basis [for administering treatments].”
Dr. Yehuda stressed that she is excited to continue this research with her team and collaborators.
“I’m excited about this team, and the fact that they have such great questions that are going to solve things that we haven’t been able to solve before, like how to prevent PTSD and identifying the drivers of these biological differences,” she shared. “I’m just happy that we were able to start something that doesn’t need to end. I have so much gratitude for the New York Stem Cell Foundation, for Kristen and her team, and for other collaborators at Mount Sinai. My clinical team are some of the most excellent and compassionate PTSD providers who can actually get the trust of our combat veterans to participate in this kind of research. So I’m very grateful to everyone.”

