Experts Explore the Power of Artificial Intelligence in Brain Disease Research
News VideoHow is artificial intelligence (AI) augmenting and improving disease research? A group representing several facets of the disease experience recently gathered to discuss how new research approaches using AI can shed light on diseases of the brain.
The engaging session, featuring Vikram Khurana, MD, PhD (leading physician-researcher at Harvard Medical School and a NYSCF – Robertson Stem Cell Investigator), Leena Panwala (President and co-founder of the INADcure Foundation), Daniel Paull, PhD (NYSCF Senior Vice President of Discovery and Platform Development), moderated by Raeka Aiyar, PhD (NYSCF Vice President of Scientific Outreach), and hosted by Susan L. Solomon, JD (NYSCF CEO), explored why it is so challenging to understand and treat brain diseases, what AI approaches are revealing about these diseases (including our new study of Parkinson’s), and how NYSCF’s integration of AI and stem cell technology is paving the way for new, effective treatments.
What makes brain diseases so hard to study and treat?
People with neurodegenerative diseases grow up developing normal nervous systems, but at some point in their life, something triggers dysfunction and loss of brain cells, leading to a progressive decline in brain function. Some neurodegenerative diseases are monogenic, or caused by a single genetic change; however, most neurodegenerative diseases are complex, meaning their exact cause or combination of causes is not well understood.
“Unlike monogenic diseases, most Parkinson’s and Alzheimer’s patients have a complex origin, which means we don’t know exactly what the genetic cause is,” said Dr. Khurana. “We make an assumption that it is made up of different genetic and environmental factors.”
A fundamental challenge for all neurodegenerative disease research is the lack of models that can recreate the disease at a given point in time, especially early in the disease course. Moreover, the traditional research approach relies on animal models, which may not accurately represent how a disease manifests in human patients.
Stem cell models of disease, however, combined with other advanced technological approaches, including genetic screening and AI, offer a better, more accurate, platform to model neurodegeneration at a given point in time, identify disease hallmarks, and test new therapies.
“If our models can be better at representing the patients that we might ultimately be treating earlier in the process, perhaps we can better capture where things might progress through the rest of the pipeline. AI can definitely help with that,” said Dr. Paull.
The complexity of neurodegenerative diseases combined with individual experiences also makes it hard to find drugs that work for everyone.
“Ultimately the problem with treating complex diseases is that patients may not have exactly the same disease,” noted Dr. Khurana. “Even in patients that have a single gene mutation that causes one of these diseases, there can be huge differences in the same family of how those patients manifest their diseases, so we need a way to classify our patients.”
“[Clinical trials may be failing] because a drug is working wonderfully for a subset of patients, but we are unable to see that because we are looking for a significant effect across a population. So we are almost always setting ourselves up for failure in these clinical trials.”
What are the unique challenges and treatment opportunities for rare diseases like INAD?
INAD is a devastating and rare neurodegenerative disease affecting very young children, which is typically diagnosed between six months to three years of age. It is caused by mutations in a single gene (PLA2G6), but presents differently in each child, and there are currently no treatments available.

“When my daughter was diagnosed with INAD, it wasn’t on anyone’s radar,” remarked Ms. Panwala. “With a global patient population of 150 children, resources weren’t really allocated to try to learn more about the disease or how to effectively treat it.”
“The NYSCF team joined me in my quest to search for treatment options for INAD. We collected skin and blood samples from multiple children affected with the disease, and created stem cells that we can use for all types of research including drug discovery.” said Ms. Panwala.
Though challenging, rare disease research also offers opportunities for larger patient populations. For example, INAD has sometimes been described as a childhood version of Parkinson’s disease. Any insights into rare diseases have the potential to alter or improve the understanding of diseases that affect much larger portions of the population.
“The fact that rare diseases could overlap with diseases that affect larger groups of patient populations is worth focusing on. If we are able to effectively treat a smaller disease group, could we then take that therapeutic to a larger patient population and effectively treat that disease as well?” said Ms. Panwala.
How does AI represent a new and exciting opportunity to improve research into brain diseases?
AI has an extraordinary ability to do what other technologies or even the best, most sophisticated scientists cannot: find patterns in massive datasets.
“As we can do bigger experiments, we’re getting more data. AI allows us to aggregate that data and look for patterns where we can apply something meaningful,” said Dr. Paull.
“Following these patients as their disease progresses generates enormous amounts of data: clinical assessments, biometrics, bioimaging.” added Dr. Khurana. “The idea that we can capture huge chunks of information that are really beyond our capacity and look for patterns with algorithms is very appealing.”
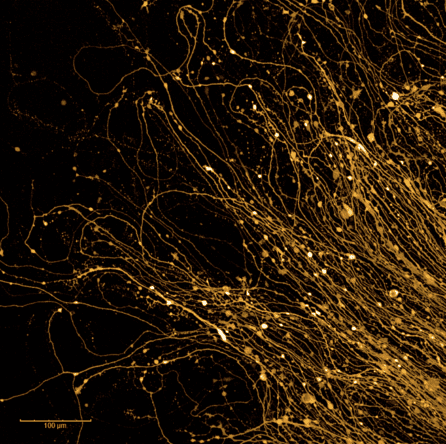
“We can take advantage of things called ‘neural networks’ that were trained on images of cats and dogs,” Dr. Paull added. “Who knew that one day they would be incredibly useful for Parkinson’s disease? Even with a giant team of people looking at the images in the way we would traditionally look at them, we wouldn’t be able to tease apart patterns the way AI can.”
How is NYSCF using AI to improve research into brain diseases?
One example of AI transforming research approaches is our recent Nature Communications study published in collaboration with Google Research, where we’ve taken advantage of the power of AI and NYSCF’s robotic infrastructure to find disease hallmarks in millions of images of skin cells from Parkinson’s patients and healthy controls. Remarkably, our models were able to identify whether a given cell image came from a healthy person or a Parkinson’s disease patient, even using skin cells.
“What was very surprising to us was that our platform could identify individuals incredibly well,” said Dr. Paull. “Even when samples from the individuals had been collected years apart, we could still tell that they had come from the same individual to begin with.”
Ensuring the research process is standardized with as little variation as possible is important for identifying trends with AI. The NYSCF Global Stem Cell Array® (our automated system for creating stem cells) helps scientists create cells and conduct experiments with the help of robots that do things the same way every time.
“If I had my coffee in the morning I might do something great, but if I’m sleepy in the evening I might not. Robots minimize this variation,” explained Dr. Paull.
At the NYSCF Research Institute, we are applying this novel approach of combining AI with our automation systems to find new and better treatments for INAD patients, in collaboration with the INADcure Foundation and patient groups.
“Using this AI-based technology, we have been able to detect disease features in INAD patients which we were not able to do in the past,” remarked Ms. Panwala. “The ultimate hope is that we can screen existing FDA-approved drugs against these cells and get to a point of having therapeutic options available to these children.”
“What is great about the INAD project is that we have also made stem cells from patients, so we can now turn them into any other cell type of interest – neurons, for example – and test if a drug is effective in that cell type,” said Dr. Paull.
Why should we be hopeful for the future?
“In the future, I foresee us looking at cells from many patients to extract these patterns and trends rather than the current process of receiving a diagnosis and everyone getting the same drug,” remarked Dr. Paull. “We will continue to try to move this forward.”
“Bringing the worlds [of clinicians and researchers] together to work on this will be very helpful,” said Dr. Khurana. “The potential here is very exciting.”
“I’m really hopeful,” added Ms. Panwala. “I’m hopeful that these breakthroughs will lead to treatment options and cures for these devastating diseases. And I think by collaborating and data sharing, we are certainly going to get there a lot quicker.”

