Experts Unpack their Groundbreaking Study of Alzheimer’s, Stem Cells, and the Aging Brain
News VideoNearly 1 in 3 seniors die with Alzheimer’s or a related dementia, yet very few treatments or preventive options are available. Understanding how exactly cells in patient brains deteriorate as they age – and how this process differs across patients – has been a major challenge.
A new study by NYSCF scientists and collaborators reveals the power of stem cell models for capturing features of aging brains in a continuum from healthy to severe Alzheimer’s disease. Experts David A. Bennett, MD (Rush Medical College, Rush Alzheimer’s Disease Center), Tracy Young-Pearse, PhD (Harvard Medical School, Brigham and Women’s Hospital) and Scott Noggle, PhD (The NYSCF Research Institute) recently discussed what their latest findings tell us about the cells in our aging brains, the genetic factors that may be driving cognitive decline, and the road toward effective treatments. The discussion was moderated by NYSCF’s Raeka Aiyar, PhD.
What makes Alzheimer’s so difficult to study and understand?
One of the most challenging aspects of studying Alzheimer’s is that scientists can’t reach into a brain and pull out cells – they have to examine tissues from deceased individuals or simulate the disease in mice.
“Alzheimer’s disease is traditionally diagnosed after death. We know that people with Alzheimer’s have an accumulation of different proteins – amyloid plaques and tau tangles – in the brain. Then, over time, patients start to lose neurons,” explained Dr. Noggle. “This problem of only being able to really know that you’re looking at Alzheimer’s after death has been something of a hindrance in trying to understand the mechanisms of the disease.”
“If you study diseases of the brain, you usually suffer from cancer envy,” added Dr. Bennett, who has been treating Alzheimer’s patients for decades. “And it’s not that you want cancer, or you want anyone else to have it. It’s just that it’s fairly easy to study relative to brain diseases. You can take the cancer out. You can look at the molecular fingerprint of the cancer. You can give somebody a drug and see how it works. The path to understanding cancer biology is much more rapid than a disease where you have to wait for people to be dead to study it.”
Researchers can insert genes into mice to give them Alzheimer’s-like plaques, but this doesn’t capture the full story.
“It’s a mouse with a human gene that causes Alzheimer’s disease,” remarked Dr. Bennett. “It bears little relationship to anything that happens on the planet naturally. We’ve cured Alzheimer’s disease in mice hundreds of times.”
Finally, Alzheimer’s is a complex disease: it’s a mix of pathologies influenced by genetics, and teasing out what causes what is a tall order.
“There’s at least a dozen different brain pathologies in your head,” noted Dr. Bennett. “Your brain, like other systems, does not want to be demented. It has ways to protect itself. When you get under the hood in the brain, Alzheimer’s disease is a very particular type of brain pathology in a sea of other brain pathologies. And you cannot separate those out in living people. You can see a couple of the pathologies, but you can’t see all of them. And you can’t see the resilience factors that are there.”
“There are people that have mutations in single genes that guarantee that they’ll get Alzheimer’s usually very early on in life, but the vast majority get Alzheimer’s very late in life,” added Dr. Noggle. “And we know that the genetics underlying our susceptibility to Alzheimer’s late in life is quite complex. And we really don’t understand how these different genetic factors combine to cause disease.”
How did the team take a new approach to studying Alzheimer’s?
This research leverages tissue samples and clinical information collected from two studies: the Religious Orders Study (ROS) and Rush Memory and Aging Project (MAP) – together called ROSMAP. ROSMAP includes thousands of participants who are tracked throughout the later stages of their life and then donate their tissues when they pass away — yielding a rich resource of clinical, cellular, and molecular data for research.
“These two cohorts are quite unique. The Religious Orders Study is a study of over 1,500 nuns, priests and brothers from across the United States and the Rush Memory Aging Project includes more than 2,200 people across northeastern Illinois,” explained Dr. Bennett.
“These studies have a couple of features that make them very different from any other studies on the planet. One is that we enroll people without Alzheimer’s, and we test them every year [to gather clinical data]. The unique feature is that participants must agree to organ donation at the time of death. So, when they die, we get their brains.”
Additionally, all of this data is being shared throughout the scientific community to accelerate progress.
“What really struck me was not only the immense amount of data that was captured from these individuals, but also the collaborative nature of the project,” noted Dr. Young-Pearse. “What makes this cohort so powerful is that all of this information acquired from hundreds of laboratories is all shared and aggregated so we can all use it to help us understand disease.”
How can stem cells be leveraged to understand this cohort?
Dr. Bennett had been collecting blood samples from ROSMAP participants for years. He and Drs. Noggle and Young-Pearse realized that with this blood, they could make stem cells, and in turn, the brain cells affected by Alzheimer’s.
“What I couldn’t believe was that we did not have stem cells from this cohort,” remarked Dr. Young-Pearse. “It’s so rich and you have living blood cells that are cryopreserved, but wouldn’t it be great to have an unlimited supply of cells from these individuals? And then even better if we could make them into any cell type in the body.”
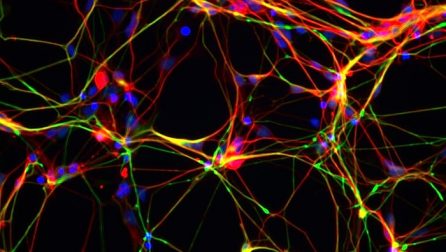
“You can’t really study the brain outside the brain, unless you [make stem cells], and that’s where NYSCF and Tracy come in,” added Dr. Bennett. “In this study, we collected blood from the participants, and we sent that to NYSCF to convert into stem cells and essentially bring it back to life. Then Tracy turns them into brain cells, and we study them to know what’s going on in the brain.”
“When we create stem cell lines from people with disease or with different diseases, we’re capturing their genetics in such a way that we can tease apart its influence,” remarked Dr. Noggle.
“There’s been at least 30 different variations of the genome that have been determined to give you some risk of Alzheimer’s disease, but it’s not clear how variations actually work in the cells that are succumbing to disease,” he continued. “Stem cells let us tease apart this cause-and-effect relationship.”
What were some of the study’s most exciting findings?
The scientists were pleased to find that characteristics found in the stem-cell-derived neurons mirrored the characteristics found in the brain tissue.
“[The stem-cell-derived neurons] have shown striking similarities to the brain tissue collected from the same individuals after they pass away,” said Dr. Noggle. “We’ve set up a platform that allows us to be confident that we’re seeing the changes that happen in the brain in the dish.”
The team also made interesting observations about how the disease affects individuals in different ways.
“One thing that I was very struck by is that when we made neurons from 50 different people and measured the amyloid plaques that the neurons made, people of different genetic backgrounds made different profiles of amyloid. It wasn’t necessarily the total amount of plaques produced that was different [between Alzheimer’s-affected and healthy individuals], but rather the types of amyloid that it made,” recalled Dr. Young-Pearse.
“We could actually see a significant association between what we were measuring in the neurons in a dish and what we could see in the brain, both the amount of amyloid plaques that were present, but more importantly, with the participant’s trajectory of cognition.”
“Some people in the cohort had very stable cognition out to a hundred years old. Some people had Alzheimer’s and a very steep decline. Some people had Alzheimer’s, but it was a relatively slow progression,” said Dr. Young-Pearse. “What was really surprising is that what we measured in the dish had some predictive value in what was observed in terms of cognition and pathology in the brain.”
“We’ve also found an interesting molecular chain of events that we think might [be involved in the disease process],” added Dr. Noggle.
“We identified an interesting connection between the amyloid plaques and the tau tangles,” remarked Dr. Young-Pearse. “There were different pathways that seemed to link the two, and one of them was this protein phosphatase that was reduced in expression when you had amyloid plaques, and that resulted in a worsening of the tau.”
“But it wasn’t in every single Alzheimer’s disease subject,” she continued. “Some subjects responded to that change in plaques by lowering this enzyme, but others were all protected from it for some reason – most likely genetically encoded. This speaks to the power of these cells for capturing the genetics and the subtle differences across humans. It also opens the door for personalized medicine.”
How will all of this inform treatment development?
“When we look at brains and look at their gene expression, we can find groups of people that fit into different buckets, or subgroups,” noted Dr. Noggle. “One of the things that I am excited to do is use these cells to understand and see if we can predict who fits in those different buckets. If you can understand what’s going on in those different buckets, we might be able to find tailored therapies, but also exclude people from going into the clinical trials in the first place, if we know the drug won’t work for them.”
Recently, the FDA approved aducanumab as a treatment for Alzheimer’s, although there has been debate as to the efficacy of the drug and speculation as to which types of patients it will help most.
“[Aducanumab] is an anti-amyloid plaque therapy that’s been approved by the FDA. It’s highly controversial, partially because the results from the clinical trial were mixed. Not everyone seems to respond to it the same way,” explained Dr. Young-Pearse. “One of the ways I would like to immediately use the cells from our study is to test whether this drug would engage amyloid plaques in a certain subset of people. That might give us some clues as to how to make it a more effective treatment.”
Altogether, the scientists are excited about what this platform will mean for personalized medicine and the future of Alzheimer’s therapies.
“It is finally a bridge to being able to do something in living people based on what we’re learning from deceased people,” said Dr. Bennett. “For somebody who’s been studying these cohorts now for over 25 years you know, I want to see that bridge. I can’t help these people anymore, but I can help their children and their grandchildren.”

