For Brain Disease Research, Patients Lead the Way
News“There are 55 million people worldwide living with Alzheimer’s or other dementias, 2.8 million living with multiple sclerosis, and 10 million with Parkinson’s,” shared NYSCF Vice President of Scientific Outreach & DEIB Raeka Aiyar, PhD. “And with our aging population, the burden of these age-related diseases is expected to at least double in the next two decades.”
How can stem cells help us to tackle this growing challenge and finally deliver effective therapies to patients? In a recent discussion featuring NYSCF Senior Research Investigator Valentina Fossati, PhD, and NYSCF – Robertson Stem Cell Investigator Vikram Khurana, MD, PhD, Chief of the Division of Movement Disorders at Brigham and Women’s Hospital and Harvard Medical School, experts shared how they are leveraging stem cells to develop personalized, patient-focused treatments for brain diseases.
“Why a patient-centric approach? One reason is that as a mission-driven, patient-focused organization, it was really important to us that today’s discussion be patient-centric,” noted Dr. Aiyar, who moderated the conversation. “Two, is because these diseases vary so greatly across patients, and therefore, three, firmly integrating the understanding of patient experiences is essential for making real progress in research.”
What compelled you to study neurodegenerative diseases with stem cells?
“Where I am – in the Ann Romney Center at Brigham and Women’s Hospital – we have hundreds of scientists working upstairs, and we see patients downstairs, which for me is a perfect setup,” remarked Dr. Khurana. “As you said, Raeka, patients are so different from each other, and that’s a huge focus of my work.”
“Brain diseases are very complex, and for me, the great draw of human stem cells was they could create this window into individual differences that occur among our patients,” he continued. “I can see patients downstairs, and I can make models of their brain disease upstairs, and that’s a very powerful way to translate findings in the lab back to patients.”
Dr. Fossati’s drive to study neurodegenerative diseases began with her own diagnosis of multiple sclerosis (MS) in 2008.
“I was newly diagnosed with multiple sclerosis, and I really wanted to find a way to leverage my background as a stem cell biologist to find a new way to study the disease,” she reflected.

Dr. Fossati wanted to turn her attention to a neglected aspect of MS and most neurological diseases: support cells in the brain called glia. And she wanted to study the disease in its native territory: human cells.
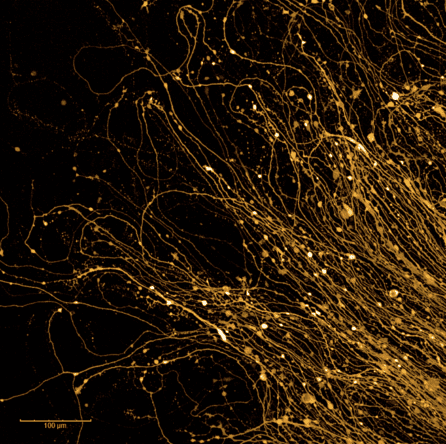
“The most vulnerable cells in MS are the oligodendrocytes, which are glial cells that generate myelin – an insulation around the neurons that is damaged in the disease,” she explained. “And so my idea was to understand and generate oligodendrocytes in a dish instead of using mouse models, because while mouse models are helpful, mice do not get MS. I spent a decade learning how to generate these cells, and now we have a collection of cells from patients that we are using to understand what goes wrong in disease.”
How are you collaborating to make a more comprehensive model of brain diseases?
“I had been focusing on neurons for a long time to study Parkinson’s, but as research evolved, it became more and more important and salient to focus on glial cells,” said Dr. Khurana. “I study a very aggressive cousin of Parkinson’s called multiple system atrophy (MSA) that is almost like Lou Gehrig’s disease (ALS). It turns out that abnormal protein changes in MSA are shared by Parkinson’s disease, and they occur in the glial cells Valentina studies.”
“So, I thought it would be fantastic to work with Valentina on this, and put our neuronal technologies together with her glial technologies to create a more comprehensive and coherent model of brain cells in the dish. And that’s what we’re doing now – we can watch how these cells talk to each other and where we can prevent its progression.”
Importantly, this system can be applied to other diseases impacted by dysfunctional proteins.
“Vik mentioned that in MSA, there is desegregation of a protein called alpha-synuclein. But there are other proteins aggregated in other diseases such as Alzheimer’s,” added Dr. Fossati. “Perhaps you’ve heard about amyloids and tau. And so when we learn how to create these protein aggregates in a dish, then it’s very easy to transfer these tools and apply them to a different disease.”
How do patients power your research?
“At heart, I’m a clinician. For me, the human stem cell work we do, and that we integrate with genetic information from patients, is an extension of my clinical interaction with the patient,” said Dr. Khurana.
“We have maybe 130 patients who have generously donated skin biopsies [from which to make stem cells], and we can follow them in the clinic, and similarly follow their stem cells in the lab. There are some very critical questions we ask in the lab that we can only identify by being very familiar with a patient themself.”
“Some patient’s disease might have started in the gut. Some might have prominent memory decline. Others have problems with blood pressure. We use an umbrella term for Parkinson’s disease, but in truth, patients are all rather different.”
“So there’s a parallel universe, if you will, between the lab and the clinic. What we are starting to do is to use patient stem cells to match a therapy to a patient. We can see if a drug shifts a patient’s trajectory. I wouldn’t have dreamed even a few years ago that we would be doing this already, so it’s a very exciting time.”
“Having MS has changed the priorities and the questions that I wanted to answer,” added Dr. Fossati. “The main problem with MS, or any neurodegenerative disease, is that everyone is different. People want to know if they can have a baby, if they can work, if they can travel. I think the only way to understand and answer these questions is to study human cells.”
One of Dr. Fossati’s ongoing collaborations is with researchers and clinicians at Johns Hopkins School of Medicine, in which stem cells collected from patients across several diseases, including MS, are turned into glial cells.
“We use these recipes that we have developed over the years to generate different types of cells in the brain – oligodendrocytes and astrocytes, which are involved in neuroinflammation – and have found some specific signatures in the cells of those with MS, even without being exposed to inflammation – the traditional environment of the disease,” reported Dr. Fossati. “And that goes against the traditional view of MS, which is that immune cells infiltrate the brain and cause the damage through inflammation.”
Dr. Fossati stressed how none of this work would be possible without the support of patients.
“I really want to thank every patient who donates their cells, because I know when you go to the clinic, you have so many other things you want to focus on. But it is so critical for the research and for the future.”
How has philanthropic support brought your research closer to patients?
Dr. Khurana received the NYSCF – Robertson Stem Cell Investigator Award in 2018, which provides 1.5M in flexible funding to early-career researchers over the course of five years.
“It’s all about freedom and flexibility and doing it in real time. That’s the key, right? You want to be supported and given autonomy to take some risks,” said Dr. Khurana. “And that’s not how conventional grants work. It’s a good process, but it’s not quick and it’s not reactive. Now, when I get calls from people wanting to test a new question, I don’t have to say ‘I’d love to do that, but we’ll have to write a grant and it will take six months, plus another year to get funded.’ I can say yes right away.”

“I’ll give you a real time example: I received a call a few weeks ago about a patient I see. It was from another researcher who had sequenced their genome and found something interesting that might be involved in the disease,” he shared. “They wanted to know if I wanted to talk more about what they found, and potentially create stem cells from the patient and make sure this gene was involved. And perhaps it could be druggable. We’re now working on this, and the only reason I can do so is because I don’t have to write a grant to support this work. I have the flexibility [via the NYSCF – Robertson Investigator award].”
Dr. Fossati began her career as a NYSCF – Druckenmiller Postdoctoral Fellow in 2009.
“People might not realize how young this field is – the ability to make stem cells from skin or blood only started in 2007,” she noted. “And these awards helped fund the pioneering scientists who have pushed the field to where it is today. And the ability to be in the same community as these people and share our ideas has been absolutely critical in achieving what we have.”
How long does it take for a therapy to enter the clinic?
Dr. Khurana shared exciting news of a drug he discovered in part using human stem cells that was afforded an accelerated path to the clinic.
“We did that very first experiment, believe it or not, in yeast cells: single cell organisms that were expressing the Parkinson’s protein, alpha synuclein,” he shared. “And we identified a drug that could fix these yeast cells, but of course, we don’t want to treat yeast cells. So in parallel, we grew the human brain cells, and sure enough, the drug we discovered could also reverse the pathologies there in very complex human cells. And the timing was remarkably good. We went from a yeast cell to a clinical trial in four and a half years, which for drug discovery is a very short time. That drug is now being developed for Parkinson’s and related disorders by the company Janssen.”
How are stem cells already accelerating treatments for neurodegenerative diseases?
“When I was diagnosed, we probably had five or six drugs available,” said Dr. Fossati. “And now there are over 20 first line therapies available. There are several clinical trials for drugs that improve myelination. It’s hard to give an exact timeline, but the fact that there are several clinical trials already happening makes me optimistic. There is also potential for stem cell treatments in MS as well, which has shown some interesting results and will likely be expanded in the future.”
“There’s different types of stem cell transplantations – for brain diseases, we can crudely split it up into three types,” explained Dr. Khurana. “One is where you replace a support cell that may be secreting something that nourishes the brain and slows down degeneration. Another type is when you do bone marrow transplants to replace immune cells and stop them from attacking the brain. The third is what is happening at places like BlueRock Therapeutics, where you make neurons from stem cells and transplant them – and that’s looking interesting and safe in clinical trials.”
NYSCF – Robertson Stem Cell Investigator Alumna Malin Parmar, PhD, is pioneering a similar cell replacement therapy for Parkinson’s in Sweden.
Both the researchers are intrigued by the possibility of long term, ‘longitudinal’ studies that begin even before a patient is diagnosed, with health data collected via wearable devices (think: a SmartWatch).
“We can track all the different parameters of a person, and collect all this data from the very beginning, even when a person is healthy, and this gives you a completely different way to understand the disease, because it gives you a baseline to compare to,” said Dr. Khurana.
“That’s exactly the paradigm of our emerging clinical trials unit. We can use wearables, along with genome sequencing and stem cells to find a druggable target,” he continued. “For example, we had a young boy who was having seizures, and we identified a mutation in his genome and have been longitudinally tracking him. We built a stem cell model of his brain in the lab, and remarkably, we can see seizures in the dish, just like in his brain. By tracking him, we can conceivably ask whether a certain therapy can shift his disease trajectory.”
What needs to happen to accelerate the path to the clinic?
“We need to continue conversations between patients, patient advocates, and scientists,” remarked Dr. Fossati. “And within the lab, we need to have interdisciplinary work. Here at NYSCF, we have stem cell biologists, neuroscientists, engineers, and people of all different backgrounds working together. We also need more opportunities for conferences or places where we can meet and discuss different approaches.”
“This is an incredibly exciting time for studying neurodegenerative diseases after many, many years where we really didn’t have any potential treatments,” she continued. “Now we see new drugs on the horizon, and we need to keep our minds open and work together to get them over the finish line. And we always have to keep patients at the top of the pyramid – they have to be our priority.”
“I completely agree with all of that,” added Dr. Khurana. “I’ll speak from the chronic disease perspective and say we need biomarkers [measurable indicators of disease], because while it is becoming more achievable to create therapies, testing them is still a challenge. We need biomarkers we can track over time so we can understand whether something is working. And I think stem cells will help us get there more quickly.”

