She Took it Personally: How a Type 1 Diabetes Diagnosis Inspired Josephine Wesely to Become a Scientist
News VideoNYSCF Principal Scientist Josephine (Josi) Wesely, PhD, was probably the only kid who showed up to her doctor’s appointments with scientific papers in hand.
“I was diagnosed with type 1 diabetes when I was 10,” she shared. “When I became a teenager, I started questioning why there weren’t better treatment options and why it was that I had this disease.”
“I looked into publications and went to my doctor’s office with a bunch of questions. I would say, ‘I read in this paper that they treated this animal with XYZ, and it seemed to work.’ I wanted to know where the studies were going, what was happening, and how it could impact me. I think he was overwhelmed,” she laughed.
The doctor couldn’t give her answers she was satisfied with, and so began her journey to get the answers herself. That journey led her to science, to a PhD in biotechnology, and now to NYSCF, where she is a researcher in functional genomics.
Read on to hear from Josi about her experiences as a patient, her work as a researcher, and the potential for curing her disease.
Challenges of a Childhood Disease
Type 1 diabetes is typically diagnosed when patients are young, with the most common age being around 13-14. The last thing an eighth grader wants to think about is glucose management, especially if it could throw a wrench in the all-consuming social balancing act of being a tween.
“Your first concerns as a young patient are usually, ‘Will this affect how people view me? What will my friends think? How will this work with school?’” Josi recalled. “You are just starting to define yourself, just starting to become your own person, and here comes this big social burden. I didn’t tell my friends at first – I was very secretive. I didn’t want to be treated differently. I wanted to be like everyone else.”
For Josi, this meant sneaking off for her injections, and in turn, not managing them as well as she should have.
“You cannot properly manage your diabetes if you always have to run into a restroom to do it,” she noted. “Or sometimes I would ignore my injections for a full day just because I didn’t want my friends to see.”
“For me, the injections and blood sugar measurements themselves weren’t even the daunting part – it was the relentlessness of it: the fact that I had to do it five to eight times a day. And I had a single mom who was working full-time, so she couldn’t be there to oversee it all.”
Age helped bolster her confidence and keep her disease management on track. Advances in technology helped too.
“When I got older, I became stronger and more independent. I was more comfortable asserting that this is who I am: I have type 1 diabetes – accept me or don’t. That makes life easier.”
“How we managed diabetes got better as well,” she explained. “Smartphone apps made it easier to track your glucose levels, so I didn’t have to write it down in a notebook. Continuous glucose measurement (CGM) also became prevalent – it’s like a little sticker you put on your arm or abdomen that controls your blood sugar. It makes for less hands-on work.”
Altogether, however, Josi still thought there must be better options. When she finished high school, she didn’t necessarily know that she wanted to become a scientist, but she eventually found that it was the best way to get the answers she so desperately wanted from her doctor all those years ago.
“That’s what science is, after all,” she remarked. “It’s all about asking questions.”
A Path to a Cure
Now, Josi is a scientist herself, and she’s excited about what stem cells could mean for patients like her.
“Stem cells have the amazing ability to turn into any cell type, including pancreatic beta cells – the cells that produce insulin and that are lost in type 1 diabetes,” she said. “Here at NYSCF, and at other labs around the world, scientists are working to create functional beta cells from stem cells that could be used in cell therapies. This would really get to the root of the disease so you wouldn’t have to worry about injections anymore. You wouldn’t have to worry about having access to insulin. It could be revolutionary for both young and older patients.”
“Stem cells also let us look at the genetics of a disease and examine people across diverse backgrounds,” she added. “It makes disease biology accessible in a way it never was before. We can even create organoids [3D clusters of tissue made from stem cells] to see how cells interact in a disease.”
As a gene editing scientist, Josi studies how genetic mutations associated with disease affect a cell, and in turn, how these effects can be prevented or treated.
“We can make a modification to DNA and see how this changes the cell,” said Josi. “Is it still functional? Does it still do its job – for example: does a liver cell still metabolize as it should? So it’s a tool to investigate how our genetics influence how our bodies work.”
Josi is also using gene editing to make pancreatic beta cells created for transplantation ‘invisible’ to the immune system so that they aren’t attacked and destroyed, a critical component for type 1 diabetes cell therapies.
“We can overexpress some of the genes that we believe will help cells evade the immune system,” she noted. “It’s an exciting approach.”
Josi is thankful that she does her work at NYSCF because of its unique position in the scientific landscape and its emphasis on patients.
“NYSCF is a great place because it is so close to the patients – we form relationships with them across different diseases and really try to get to personalized medicine,” she noted. “It is very different from academic institutions, pharma, or biotech. We need all of them, but NYSCF is very unique in its focus on patients, communication, and advocacy.”
If Josi could go back and tell her newly-diagnosed 10-year-old self anything, it would be to hold out hope, and to connect with others like her, and to keep asking questions.
“If I could suggest something to my 10-year-old self, I would advise seeking out perhaps a patient support group with people my own age. I’d also suggest the same for parents, especially as they try to help a child through a disease they may not have had experience with before.”
“I’d also advise patients to keep asking questions, especially if you are like me and a doctor cannot answer them to the extent you’d like,” she added. “Find a scientist, a company that produces insulin – anyone who you think could help, and don’t be afraid to look for information.”
Finally, Josi wants everyone living with a condition like hers to know that they are not alone.
“Everyone has to deal with health issues at some point in their lives, so definitely do not give up,” she said. “I am often impressed by where I am and how things turned out, especially when I was scared for so long. I’m a mom now. I lead an amazing team. I’m doing things I love every day, and I want to empower others to do the same.”
Read more about Josi’s work and type 1 diabetes breakthroughs:
The Gist of Gene Editing: Inside Biomedicine’s Hottest Tool
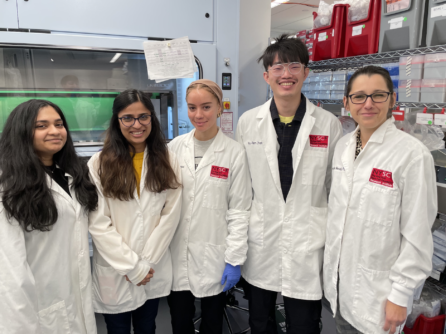
Students Explore Gene Editing and Careers in STEM
New Hope for Diabetes: A Discussion with Dr. Simi Ahmed
Progress, Challenges, and Promise: On the Road to a Type 1 Diabetes Cure
Taking on Type 1 Diabetes: Researchers and Patient Advocates Unite in the Quest for a Cure

