Envisioning a Brighter Future for Macular Degeneration Patients: Experts Unpack the Path to a Cell Therapy
News VideoAge-related macular degeneration (AMD) is a leading cause of vision loss, and those over the age of 75 have a nearly 30% risk of being affected. However, cell therapies are now offering the opportunity to restore vision in these patients by replacing dying cells with healthy ones. NYSCF and the National Institutes of Health (NIH) are currently developing a therapy that leverages the power of stem cells to do just this.
This month, Stanley Chang, MD (K.K. Tse and Ku Teh Ying Professor of Ophthalmology, Columbia University), Kapil Bharti, PhD (Senior Investigator, National Eye Institute), and Susan L. Solomon, JD (Founder and CEO, NYSCF Research Institute) discussed the therapy’s path to the clinic and why they are hopeful for the future of AMD treatments.
What causes different types of AMD?
“AMD is a leading cause of irreversible blindness in people over the age of 60,” explained Dr. Chang. “It affects women more than men because women tend to live longer than men, and by 2050, the number of affected Americans will be about 5 million.”
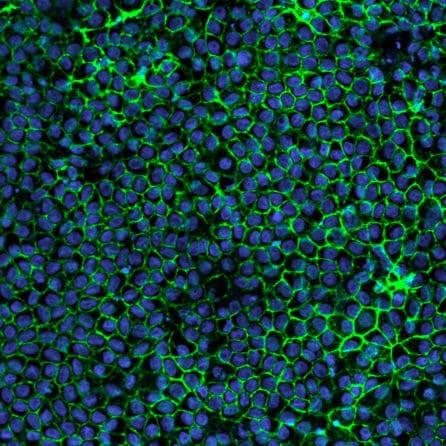
In AMD, eye cells called retinal pigmented epithelial cells (RPE cells) begin to die, resulting in a loss of central vision.
“Macular degeneration is broken up into two types: the first is dry AMD, where there’s a degenerative process causing atrophy of the RPE cells and the visual acuity loss tends to be relatively slow,” said Dr. Chang. “The second is wet AMD, where there is leakage from blood vessels under the retina, and this causes fluid to leak and sometimes bleed, resulting in loss of transparency of the retina.”
“Both types of AMD can cause loss of reading vision and central vision, and about 8-20% [of patients] convert from dry to wet macular degeneration,” he continued. “We also know that even with long-term treatment of wet macular degeneration, patients can lose further vision from the dry component of dry macular degeneration. “
What current treatments are there for wet and dry AMD?
Wet AMD is most commonly treated with periodic injections of an antibody drug called an “anti-VEGF,” which helps prevent abnormal blood vessel growth and stop the bleeding that damages RPE cells.
“The current treatment with intravitreal injections of medications have become the most frequently performed eye procedure globally: it is done in about 10 million Americans a year,” said Dr. Chang. “The problem with current [wet AMD] treatments is that we have to bring the patient back every 4-8 weeks for the treatment, which carries about a 1 in 1,000 risk of infection. So over a patient’s lifetime, the risk of infection is pretty significant. After long periods of treatment, patients may also lose their visual acuity from the progression of dry macular degeneration.”
The outlook for dry AMD is even worse, as there are no effective treatments to slow, reverse, or prevent the disease.
“There is currently no good treatment for dry AMD. So far, the only treatment is vitamins, and they probably do not have a strong effect on treatment.”
Why treat AMD with a cell therapy?
Unlike current treatments, which aim to slow progression at best, a cell therapy may offer actual restoration of function.
“Stem cell treatments offer the possibility of actually improving vision,” noted Dr. Chang. “I think this [therapy] offers the opportunity to really change the way we can treat these patients, because the late stages of macular degeneration, whether it’s dry or wet, can really cause people to lose their ability to function, to socialize, to recognize people. They’re unable to read. They’re unable to drive. They feel isolated. The loss of sensory input may accelerate dementia. There are many of my patients who have end-stage disease who complain of hallucinations…They’re just struggling to maintain some quality of life.”
“One of the exciting things that we have to draw on is Pete Coffey [2011 NYSCF – Robertson Stem Cell Prize Recipient] who showed that RPE cells derived from stem cells could restore vision to the point where patients were able to regain their drivers licenses,” noted Ms. Solomon. “But there is still a ways to go until this becomes a standard of care.”
How will NYSCF’s AMD therapy work?
For NYSCF’s therapy, which targets dry AMD, scientists will create healthy RPE (RPE) cells (the cells lost in the disease) from stem cells derived from a patient’s blood, which will be placed onto a specially designed patch and surgically implanted behind the retina by surgeons at Columbia University – NY Presbyterian Hospital led by Dr. Chang and colleagues. The RPE patches will be created using a method established by Dr. Bharti that is being used in a clinical trial currently enrolling patients with AMD.
A major benefit of this approach is that it is autologous, meaning the cells are derived from the patient themself rather than a donor, reducing the likelihood of the patient’s immune system attacking the transplanted cells and eliminating the need for immunosuppressants, which can cause side effects like increased risk of infection, nausea, and loss of appetite.
“The advantage of an autologous tissue would be that it’s immune-compatible; it comes from a patient’s own tissue,” remarked Dr. Bharti. “And that means we don’t have to give them any immunosuppression during or after the surgery. And as [Dr. Chang] would tell you, these are often older patients who can have bad reactions to immunosuppressants. So by doing this autologous process, we avoid all of those adverse events.”
Why is the eye a good place for a cell therapy?
Stem cell therapies for a variety of diseases are still relatively new, and the eye could serve as an ideal target to start with in part because of its ‘immune privilege’ and its accessibility for both surgery and monitoring effectiveness over time.
“There’s something called immune privilege, where in certain spaces, the immune system doesn’t attack tissue that isn’t natural,” explained Dr. Chang. “And we’re putting in iPS [induced pluripotent stem cell]-engineered cells from patients themselves, so they hopefully [carry] the patient’s histocompatibility factors, and they won’t be recognized by the eye.”
“Once [the patch] is in the eye, you can see what’s going on much better than any other organ transplant into the body, where you would need an x-ray,” said Dr. Chang. “With our technology, we have the resolution to look at micron [one millionth of a meter] changes so that we can see early changes and detect them before the patient even might have any symptoms.”
What will the surgery be like?
“The surgery will be done as an outpatient under local anesthesia,” explained Dr. Chang. “We would do a normal vitrectomy [in which the vitreous humor gel that fills the eye cavity is removed to provide better access to the retina], and use an instrument to insert this layer of cells directly under the macula. A small cut would be made into the retina and this sheet of cells would be slid under the macula.”
“It will take, I estimate, between one and two hours,” he continued. “With experience, we could probably do it in an hour, but with the first few cases we would probably take a little longer – an hour and a half or so – to make sure everything is done properly.”
What are the biggest challenges in developing and implementing this therapy?
One challenge in developing this kind of therapy is determining how to scale up and ensure cells are manufactured properly.
“We’re still learning a lot about these cells: how to quality control them and make sure that we are delivering the right kind of cells, but also how to really make this a widely available technology,” explained Dr. Bharti. “We would need to make the manufacturing process consistent across multiple sites. If you want to do it at twenty different places within the country, how can we make sure that it’s consistent? So factoring in things like automation, removing subjectivity, using artificial intelligence to QC to all of this will not only make it more streamlined and successful, but also reduce the cost as we move toward live transplants.”
Dr. Bharti is also working on a surgical tool to aid in the implantation procedure.
“We are working on a preloaded RPE patch and a surgical delivery tool that is frozen so when it reaches the surgeon, all they have to do is thaw it, check that it’s intact, and then transplant it,” he added.
Dr. Chang stressed that we cannot be 100% sure that the new cells won’t be degraded by the same processes that degraded the original cells.
“How do we know that these cells are going to survive?” he asked. “That’s the biggest challenge for us as clinicians and scientists, because the cells started degenerating for some reasons that we don’t completely understand. So when we put a new, healthy, young layer of cells back into the eye, are they going to survive? “
However, previous studies suggest that the implanted cells should stay healthy for a while following the procedure.
“For the work we’ve done in animal models, we’ve managed to keep these cells alive for months, and these are foreign [human] cells in animals, so the animal’s immune system is trying to attack them,” said Dr. Bharti. “And despite that, for months we could keep the cells alive. Additionally, if you look at the early proof-of-concept surgical procedures where people would cut out RPEs from the periphery of the same eye and translocate them into the area of damage, they saw that when the transplants were successful, those cells survived for years. I think that provides the proof-of-concept that stem cell transplants, if delivered correctly, would have a fighting chance of surviving in [the eye].”
How soon will we know if the therapy works?
While a therapy at the National Eye Institute fueled by Dr. Bharti’s studies is already in Phase 1, NYSCF is still working toward Phase 1. This phase of a clinical trial tests for safety and feasibility, so efficacy results may not be immediate.
“These are Phase 1 safety and feasibility trials in early patients, so we are only going to be looking to see that the cells are safe and it’s feasible to do it,” noted Dr. Bharti. “We can follow these patients for a while to make sure the cells are alive and they’re not causing any harm. I think it would be too premature to say the cells in dry AMD patients will immediately start showing any signs of recovery.”
Who would be eligible to receive this therapy?
Initial clinical trials likely won’t include patients who would be at a higher risk due to advanced age or underlying conditions, but this doesn’t mean those people would be excluded in later stages once the therapy is proven safe.
“At this stage we’re being careful at the first few patients because we don’t want any confounding factors interfering with our outcome variables,” said Dr. Bharti. “But I think as we move forward, if we have demonstrated that the transplant is safe and we can actually do it, I think we can easily offer it to a broader population of patients.”
Will this be a one-and-done therapy?
The panelists hope this therapy will offer a one-time cure for dry AMD. For patients who have lost cells other than RPEs such as photoreceptors (cells that make color and night vision possible), Dr. Bharti is working on adding those cells into the mix to provide a comprehensive treatment.
“We are hoping that this is a one-and-done [therapy]…Whether it will restore vision completely will depend on where we transplant, because if the photoreceptors are already gone, an RPE transplant is not going to cover that,” he explained. “So for the future, we are working on developing a dual RPE and photoreceptor ‘sandwich’ transplant with partners at the University of Wisconsin, Madison.”
Are there any risks or downsides to a cell therapy for AMD?
“The risk always stays until we have proven that the cells are safe,” said Dr. Bharti. “There is a risk, of course, of the procedure. It’s not a simple injection. Like [Dr. Chang] showed, it’s a little bit more than a minimally invasive procedure. There are some risks associated with giving immunosuppression, which we took out by using autologous transplant, but [induced pluripotent stem cells] themselves have risks: what if their genome is unstable and they become oncogenic? We’ve rigorously designed many tests for this. We transplanted [the cells into] so many animals to demonstrate to the FDA that the cells do not become tumorigenic and are not toxic, but that result was concluded using animals. Until we do the first few patient transplants, we’ll never be sure that this transplant is safe, so that inherent risk is there. But I think we are doing the right science and letting the science guide the safety of the transplant.”
Dr. Chang expressed that the other risks are standard for eye procedures.
“The risk of the procedure is maybe one 2,500 of infection, which was the typical infection rate,” he said. “After vitrectomy, the other [risk] would be retinal detachment. In general, that can be repaired, however.”
Why should we be optimistic about this therapy?
“In my view, this is clearly going to bear fruit for patients, and I’m incredibly excited about it,” remarked Ms. Solomon.
“When you think about the history of medicine, transplantation has revolutionized what we can do for patients,” said Dr. Chang. “And so this is just another step of the transplantation process, a microcosm of large organ transplantation in that you’re transplanting a layer of cells, and we actually regenerate [cells to stop] abnormal function. So I’m pretty excited about the technologies and hopeful that it will give some regenerative capacity for our patients and restore quality of life.”
“I couldn’t agree more,” added Dr. Bharti. “I think regenerative medicine is at a crossroads and we have built a critical mass through enough proof-of-concept studies that we can do this, especially in the eye with RPEs. In the last couple of years, venture capitalists and pharma have invested billions of dollars in regenerative medicine because it will transform all these diseases that we haven’t been able to treat so far. To me, that’s really promising.”

