Updates on the NYSCF Community’s Fight Against COVID-19
We are proud of our scientists and Innovator community who are hard at work developing solutions for those impacted...We are proud of our scientists and Innovator community who are hard at work developing solutions for those impacted by COVID-19. This ranges from better diagnosing the SARS-CoV-2 viral infection that causes the COVID-19 disease, to developing effective treatments and vaccines, to protecting healthcare workers on the front lines. Read below about current COVID-19 projects and check back for regular updates on this promising work.
Latest conversation with COVID-19 experts
Watch a panel discussion (or read highlights here) held on June 10, 2021 to hear from experts about how we can reach herd immunity, both locally and globally, and navigate the future of this pandemic.
Watch previous discussions held on August 27th, May 20th, and April 23rd (2020) and check out our vaccine series for information on vaccine development and rollout.
NYSCF Research Institute Making Lung Cells for COVID-19 Research
We are leveraging the power of human stem cells as disease models to help better understand COVID-19 and find urgently needed treatments, in collaboration with top scientists worldwide. Led by NYSCF’s Senior Vice President of Research Scott Noggle, PhD, we are using stem cells to create the specific types of lung cells that are affected by COVID-19.
We are generating these lung cells using our extensive, genetically diverse biobank of human induced pluripotent stem cell lines, and make them available to the broader scientific community as a resource for COVID-19 research. Our goals in creating these models are to accelerate studies of how the SARS-CoV-2 virus infects and affects lung cells, how genetics may make certain individuals more susceptible to severe cases of the disease, and to test therapies with the potential to stop or prevent infection. These lung cell models of COVID-19 will be used by leading virologists and chemists across the globe, including:
- NYSCF–Robertson Investigator Alumna Shuibing Chen, PhD, of Weill Cornell Medicine
- NYSCF – Druckenmiller Fellow Alumnus Larry Luchsinger, PhD, of the New York Blood Center
- Adolfo Garcia-Sastre, PhD, Director of the Global Health and Emerging Pathogens Institute of Icahn School of Medicine at Mount Sinai
- Sumit Chanda, PhD, Director of the Immunity and Pathogenesis Program, Sanford Burnham Prebys Medical Discovery Institute
- Nevan Krogan, PhD, Director of the Quantitative Biosciences Institute, University of California San Francisco
Feng Zhang Develops CRISPR-Based COVID-19 Diagnostic Protocol and Launches Survey for Hotspot Detection

NYSCF – Robertson Stem Cell Investigator Alumnus Feng Zhang, PhD, of the Broad Institute of MIT and Harvard, is using his CRISPR gene editing-powered tool called SHERLOCK to develop a paper strip test that can quickly and inexpensively detect the virus. This tool has recently received emergency authorization from the FDA to be used by “high complexity laboratories” as a diagnostic.
Dr. Zhang has also introduced a procedure for better extraction of RNA from patient swab samples, which has been a bottleneck for SARS-CoV-2 testing.
Mass population survey efforts are underway to allow early detection of COVID-19 hotspots, including an app called ‘How We Feel‘ deployed by Dr. Zhang, and a web survey and dashboard showing county-level data from the Englander Institute for Precision Medicine at Weill Cornell, directed by Olivier Elemento, PhD, a member of the NYSCF Women’s Reproductive Cancer Initiative Scientific Advisory Board.
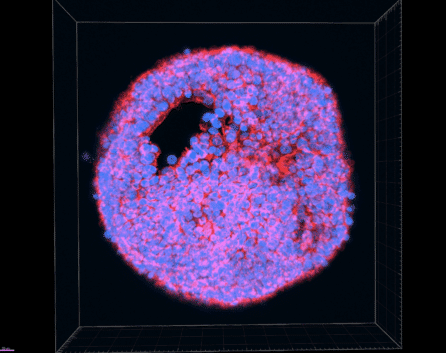
Shuibing Chen Testing COVID-19 Drugs Using Stem Cell Models of SARS-CoV-2 Infection

NYSCF – Robertson Stem Cell Investigator Alumna Shuibing Chen, PhD, at Weill Cornell Medicine, is testing drugs on the human cells susceptible to SARS-CoV-2 infection.
Dr. Chen is creating organoids (3D clusters of human tissue made from stem cells) that contain cells believed to be most susceptible to SARS-CoV-2 infection. She is using these stem cell models of the infection to test which drugs may help combat the disease. In papers published in Cell Stem Cell and Nature, Dr. Chen has established powerful stem cell models of SARS-CoV-2 infection in a variety of cell types (including pancreas, liver, heart, and neurons) and evaluated the ability of 1,280 FDA-approved drugs to block SARS-CoV-2 entry into human cells. In later stages of this research, she will use NYSCF’s automated technologies to scale up and accelerate her drug screens.
Larry Luchsinger Searches for Indicators of Severe Reaction to COVID-19

NYSCF – Druckenmiller Fellow Alumnus Larry Luchsinger, PhD, at the New York Blood Center, is collecting samples from recovered COVID-19 patients and examining them for biomarkers (molecular signatures) that indicate an increased risk of severe reaction to the virus. This work may lead to a future test for predicting disease severity.
NYSCF Research Institute scientists are working with Dr. Luchsinger to develop and implement best practices for analyzing these large clinical datasets.
His team recently released the results of a study on a rapid antibody test submitted to the FDA for approval.
Biotech Founded by Derrick Rossi Launches Clinical Trial for New Vaccine

Moderna Therapeutics, a biotech founded by NYSCF – Robertson Stem Cell Investigator Alumnus Derrick Rossi, PhD, has produced a SARS-CoV-2 vaccine proven generally safe and shown to be effective in preventing COVID-19 in clinical trials. Moderna’s vaccine was first to enter clinical trials,just 63 days after SARS-CoV-2 was sequenced – an unprecedented feat. The two-dose vaccine was 94.1% effective based on a total of 196 cases of symptomatic COVID-19 occurring in the company’s 30,000-volunteer study, and is currently awaiting Emergency Use Authorization by the FDA.
Moderna’s innovative vaccines use engineered messenger RNA molecules that instruct cells to produce specific proteins, based on a technology pioneered by Dr. Rossi. The company’s messenger RNA medicines prompt the body to produce the proteins that are missing, dysfunctional, or therapeutically useful in a disease.
Deepta Bhattacharya Develops Test for Detecting Antibodies Against COVID-19 in Recovered Patients

University of Arizona researchers co-led by NYSCF – Robertson Stem Cell Investigator Alumnus Deepta Bhattacharya, PhD, have begun using a test that can detect antibodies against the COVID-19 virus in previously infected people. The tool will help researchers better understand how widespread the virus is, whether someone can become reinfected, and how to advance vaccines and treatments for the disease.
The test works by measuring the presence of antibodies specific to the SARS-CoV-2 virus in a person’s blood. Even if a person doesn’t show symptoms of COVID-19, they can still have antibodies in their blood if they were previously infected. And if scientists can determine which antibodies helped that person fight off the virus, they can mass-produce them for use in treatments and vaccines.
“One of the goals of what Janko and I would like to do is from these patient samples, figure out which specific antibodies are protective,” Dr. Bhattacharya told The Arizona Republic. “Then that actually can be something that is therapeutically useful.”
Dr. Bhattacharya is also studying the body’s immune response to SARS-CoV-2, finding that immunity appears to be stable for several months following infection.
“The antibodies decline, but they settle in what looks like a stable nadir,” which is observable about three months after symptoms start, Dr. Bhattacharya told The New York Times. “The response looks perfectly durable.”
Chris Gregg Using Artificial Intelligence to Accelerate Diagnosis

NYSCF — Robertson Investigator Alumnus Chris Gregg, PhD, is adapting his artificial intelligence-based Storyline platform – a platform for analyzing cognitive and behavioral patterns where patients can answer questions about their disease experience over time – to collect and analyze comprehensive symptomatic data from potential COVID-19 patients to accelerate diagnosis.
Stephen Brohawn and Hillel Adesnik Searching For New Drug Targets

SARS-CoV-2 viruses (and all human coronaviruses) encode two essential ion channels in their genomes called E and 3A. Disruption of either channel reduces virulence and disease in animal models, making them promising, albeit understudied, targets for antiviral therapeutics. NYSCF – Robertson Neuroscience Investigators Steve Brohawn, PhD, and Hillel Adesnik, PhD, are using high-throughput drug screening approaches to identify novel inhibitors of E and 3A channels. This will be complemented by studies to understand precisely how these channels function and how they can be blocked by small molecule drugs.
Ed Boyden Developing Electricity-Free Ventilators, New Detection and Intervention Strategies

NYSCF – Robertson Neuroscience Investigator Alumnus Ed Boyden, PhD, of MIT is spearheading a number of projects aimed at better detection and treatment of COVID-19.
Dr. Boyden and collaborators have developed a prototype of a ventilator, based on initial designs by Dr. John Dingley, that does not require electricity or batteries to run. It is instead fueled by pressure from the ventilator’s oxygen tank, allowing greater portability for these essential devices.
His team is also developing an inhalable therapeutic that would block the ‘doorway’ that SARS-CoV-2 uses to enter human cells as well as a gene therapy that introduces a ‘dummy’ virus into the body to prevent SARS-CoV-2 from replicating.
Additionally, two of Dr. Boyden’s postdocs are developing a handheld diagnostic device to detect SARS2-CoV-2 at point-of-care based on its RNA sequence. This diagnostic builds on an existing genetic analysis device that can be used to validate the identity of wildlife or food products.
Claire Wyart Launches Website with COVID-19 Information From Experts

NYSCF – Robertson Neuroscience Investigator Alumna Claire Wyart, PhD, of the Brain and Spine Institute in France is working with experts in virology, epidemiology, and immunology on a website called ‘Adiós, Corona!’ that provides helpful tips and information on testing, distancing, transmission, and much more. The site aims to establish best practices to stop the spread of the virus and help the public stay safe. Scientists are currently working to translate the site into several languages, including English, Spanish, French, Italian, Arabic, Russian, Portuguese, Greek, and Turkish.
Jay Rajagopal Exploring the Susceptibility of Different Tissues to Infection
NYSCF – Robertson Stem Cell Investigator Alumnus Jay Rajagopal, MD, of Harvard Medical School, is studying which tissues are most susceptible to SARS-CoV-2 infection and what puts some people at increased risk of a severe reaction. His group analyzed information gathered through a consortium called the Human Cell Atlas Project that collects and centralizes data on various cell characteristics, many of which are relevant to disease. The study appears in Cell.
“[By examining data from] millions of cells, we could correlate expression [of certain features] to clinical findings,” he explained during a panel discussion at the 2020 NYSCF Conference. “For example, it came up epidemiologically that age, gender, and smoking status seem to affect the course of COVID-19, and all of that started to make sense based on [what we saw] in the lung cells.”
Mitch Guttman Discovers How SARS-CoV-2 Shuts Off the ‘Alarm System’ in Human Cells

Infection with the SARS-CoV-2 virus suppresses several critical defense functions used by human cells to fight off viruses, effectively disabling the cell’s ‘alarm system,’ finds a new study in Cell by NYSCF – Robertson Stem Cell Investigator Mitch Guttman, PhD, of the California Institute of Technology. This study sheds light on several specific ways that the SARS-CoV-2 virus disrupts the function of human cells, providing a framework for studying emerging viruses and clues for therapeutic efforts.
Justin Ichida Looking for Drugs that Prevent Infection

NYSCF – Robertson Justin Ichida, PhD, of the University of Southern California is working to understand if a class of drugs called ‘kinase inhibitors’ can protect stem cells in the lungs and other organs from SARS-CoV-2 infection.
Kristen Brennand and Takanori Takebe Exploring How Genetics Impact COVID-19 Susceptibility

NYSCF – Robertson Stem Cell Investigator Alumna Kristen Brennand, PhD, of the Icahn School of Medicine at Mount Sinai, and NYSCF – Robertson Stem Cell Investigator Takanori Takebe, MD, of Cincinnati Children’s Hospital are using stem cells to explore how our individual genetics make us more or less susceptible to SARS-CoV-2 infection.
José Ordovás-Montañés Pinpoints Which Cells SARS-CoV-2 Infects and How the Virus May Hijack One of the Body’s Defense Mechanisms

Research led by NYSCF – Robertson Stem Cell Investigator José Ordovás-Montañés, PhD, of Boston Children’s Hospital pinpoints the likely cell types that SARS-CoV-2 infects and shows that a process meant to protect cells from infection may be helping the virus gain entry. The work appears in Cell.
Kay Unger Mobilizing Fashion Industry to Deliver Personal Protective Equipment to Hospitals

NYSCF Board Member Kay Unger, a pioneer in the fashion industry, is working with leaders in the fashion industry to increase the production and distribution of essential personal protective equipment (such as masks and gowns) for healthcare workers.
Francesco Clark Producing Hand Sanitizer for Hospital Workers

NYSCF Board Member Francesco Clark, founder of Clarks’ Botanicals, is mobilizing his company’s manufacturers to produce hand sanitizer. The sanitizer is available for purchase at the exact cost of production, and Mr. Clark is working with Montefiore Medical Center in the Bronx to donate 5% of total production to hospital workers.
NYSCF Research Institute 3D Printing Personal Protective Equipment for Healthcare Professionals
Our scientists and engineers are using 3D printing technology to create personal protective equipment, such as protective visors, for New York–based healthcare professionals currently experiencing shortages.


