Translational Research Takes Center Stage at NYSCF Conference
News“Medicine shouldn’t be one size fits all,” National Institutes of Health (NIH) Director Dr. Francis Collins told the audience of the NYSCF Conference last week. “Think about it this way: we don’t give everyone with poor eyesight the same glasses prescription. Patients heal best when we consider their individual differences.”
This concept is called precision medicine, and it is just one of the many groundbreaking advancements being accelerated by stem cell research. Precision medicine boils down to getting patients the right treatment at the right time. With patient-specific stem cells, we can delineate the genetic and molecular characteristics that underlie a patient’s unique disease experience, allowing us to create targeted treatments. At the thirteenth annual NYSCF Conference – a two-day meeting on translational stem cell research featuring presentations and discussions from the world’s top stem cell scientists and leaders held at The Rockefeller University – the progress towards precision medicine was striking.
The NIH is helping drive this progress as part of its Precision Medicine Initiative, which aims to understand how a person’s genetics, environment, and lifestyle can help determine the best approach to prevent or treat disease. Dr. Collins spoke about one program within this initiative called All of Us – an effort to build a national research cohort of one million or more participants that is now open for enrollment. The idea is that the more information we have about the diverse genetic blueprint, the better we can detect patterns behind how disease is acquired and inherited.
Precision medicine was just part of the picture at the conference. Stem cells are revolutionizing biomedical research in three main areas: disease modeling, drug testing, and cell replacement therapies. NYSCF is committed to advancing all three of these areas, and the conference speakers showcased exciting new findings in each.
Making a “Disease in a Dish”

The University of California, San Diego’s Dr. Kelly Frazer uses stem cells to understand the genetic and molecular basis of disease progression. In a panel discussion entitled, “Resolving Disease Genetics Using Stem Cells,” Dr. Frazer spoke about how this concept can be applied to cardiovascular disease alongside NYSCF Senior Vice President of Research Dr. Scott Noggle and NYSCF Scientific Advisor and Harvard Associate Professor of Stem Cell and Regenerative Biology Dr. Kevin Eggan, moderated by NYSCF–Robertson Investigator Dr. Kristen Brennand of the Icahn School of Mount Sinai.
Dr. Frazer explained that heart cells created from stem cells reveal early developmental defects that lead to disease in adulthood. Such defects might be harder to detect later in life through biopsies– but by studying developing cells in a dish, we can catch a glimpse into the mechanisms driving the disease, possibilities for early diagnosis, and hopefully early intervention in disease progression.
Dr. Collins hopes that stem cell models of diabetes will help further our knowledge about its genetic basis.
“Examining how patient beta cells behave is a great opportunity for studying diabetes,” explained Dr. Collins. “My lab is collaborating with NYSCF to create beta cells from the stem cells of patients with type 2 diabetes, giving us a glimpse into its possible genetic causes.”
The genetics behind type 2 diabetes have traditionally been difficult to elucidate, and the team hopes this project will help us better understand the ways in which the disease can run in families and why it can often appear sporadic.
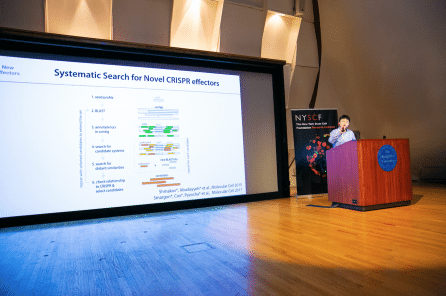
The potential to understand disease genetics using stem cells has been transformed by CRISPR gene editing, which allows researchers to precisely introduce or correct disease-associated genetic mutations and measure their impact. Since the CRISPR/Cas9 system originated from the bacterial immune system against viruses, one of its pioneers, MIT Professor of Brain and Cognitive Sciences and Biological Engineering and NYSCF – Robertson Stem Cell Investigator Dr. Feng Zhang, believes the keys to the next revolutionary molecular technologies may be held by the vast diversity of microbes on earth. His lab has discovered other microbial enzymes capable of performing useful functions, such as editing RNA with applications in therapeutics, and nucleic acid detection with applications in diagnostics – and the search continues.
One of the biggest revolutions in disease-in-a-dish modeling has come from organoid technology: 3D aggregates of brain tissue made from stem cells. By providing an environment for cells to interact the way they would in an actual human brain, brain organoids allow researchers to observe brain development, study disease, and test promising new drugs.
For organoids to faithfully recapture brain and disease biology, a major challenge has been their reproducibility. NYSCF–Robertson Stem Cell Investigator Alumna and Chair of The Harvard Department of Stem Cell and Regenerative Biology Dr. Paola Arlotta demonstrated unprecedented consistency of organoid composition across samples, opening the door for more detailed and accurate research into brain development and disease.
“We dream of the day that we can study human neural circuits in response to stimulation or in the context of complex genetics,” said Dr. Arlotta. “The potential of brain organoids to become a real experimental system is high, but we must focus on controlling cell variability.”
Yale’s Dr. Stephen Waxman is using stem cells to model “pain in a dish” by focusing on a rare, debilitating disorder called erythromelalgia, or “Man on Fire Syndrome.” In this condition, even the slightest warmth causes an extreme burning sensation in the hands and feet—leaving patients in excruciating pain. Unfortunately, these patients are also typically resistant to treatment.
“One day it would have sounded like science fiction to model pain using stem cells,” said Dr. Waxman. “But we have managed to do it by taking stem cells from patients with the disorder, turning them into sensory neurons—the cells that help us feel pain—and then studying their activity.”
Stem Cells & Drug Testing
With ‘pain in a dish’, Dr. Waxman was able to study the activity of sensory neurons and identify a drug that kept them from firing too much (a possible cause of the burning sensation the disease causes), theoretically relieving the simulated “pain” in the dish. When tested in patients, the drug worked: their pain was reduced. And beyond treating man on fire syndrome, Dr. Waxman’s study has broader implications for alleviation of chronic pain, serving as a model for how to develop and test potentially non-addictive opioids.
Like Dr. Collins, Weill Cornell Medical College’s Dr. Shuibing Chen, a NYSCF–Robertson Stem Cell Investigator Alumna, is studying diabetes. She is making patient stem cells into pancreatic beta cells to resolve the genetic and environmental factors that influence their behavior and to identify drugs that correct their dysfunction.

Her team looked at one of the two genes that are known to play a role in type 1, type 2, and neonatal diabetes, finding that cells carrying this mutation had trouble developing into beta cells and were more likely to die if they did make it to this stage. The team then tested a drug on the developing cells and found that it was able to rescue the beta cells from dying both in the dish and in an animal model—an exciting result that suggests it could one day be used as a therapy for genetic forms of the disease.
Google’s Philip Nelson also hopes to successfully identify characteristics of disease and test new drugs. In his collaboration with NYSCF, his team is using a unique tool to understand how cells dysfunction: machine learning.
“Machine learning can help us look at a cell, identify markers that indicate disease, and then apply this information to other cells,” he says. “The algorithm improves upon itself and makes sense of lots of existing data to make predictions about new data.”
The information we gather using machine learning will help us understand how cells change in disease, and then identify drugs that revert them back to normal— a central goal of the project.
Cell Replacement Therapies
The ability of stem cells to become virtually any cell type in the body means that they also have the potential to replace the cells that are lost in degenerative diseases. Many such approaches are now moving towards the clinic, and FDA’s Director of the Center for Biologics Evaluation and Research (CBER), Dr. Peter Marks, spoke about the FDA’s efforts to accelerate their approval as therapies.
“Our job is to help move treatments forward,” Dr. Marks explained. “With stem cell therapies, that means making sure there are standards for reproducible production and manufacturing, as well as early planning about how to scale up.”

Fittingly, the final two presentations of the conference highlighted two prospective cell replacement therapies about to enter phase 1 clinical trials.
Dr. Kapil Bharti, head of the National Eye Institute’s Ocular and Stem Cell Translational Research Unit at the NIH, is testing a therapy that targets cells in the retina that die due to macular degeneration. By implanting a patch containing non-diseased cells into the eye, the healthy replacements have shown promise for integrating into their surrounding environment and restoring vision.

Dr. Lorenz Studer, Director of Memorial Sloan Kettering’s Center for Stem Cell Biology and a founding member of NYSCF’s Medical Advisory Board, is using stem cells to create new dopamine neurons (the cells lost in Parkinson’s disease) that can be transplanted into patients, replacing the damaged cells and stimulating normal dopamine signaling within the brain.
“These cells have the potential not only to replace the dopamine neurons that are dying in Parkinson’s disease, but to reconnect within the brain and make sure the right cells are receiving the dopamine they need,” said Dr. Studer.
With so many revolutionary advancements taking place in labs around the world, it is understandable why Dr. Studer is optimistic about the future of stem cell research.
“We’ve already seen the incredible feats we can accomplish with stem cells, and now treatments are starting to reach patients,” said Dr. Studer. “I’m excited for the coming years because I think we’ll have an even better understanding of what stem cells truly can do and the mysteries we can solve with them.”
At the forefront of the next wave of discoveries are the field’s young scientists. The conference’s poster session served as a forum for this group to showcase their work, and it was a very impressive and competitive competition. This year’s winner was Görkem Garipler of New York University, with a poster on how gene editing can be used to identify factors that help cells maintain their pluripotency, and the runner up was Manasa Srikanth of the University of Maryland, with a poster on the molecular basis of Gaucher disease. With so many bright and enthusiastic young scientists entering the field, it is sure to be only a matter of time before even more therapies reach patients.