Variants vs. Vaccines: Ending the Pandemic in the US and Worldwide
In the United States, COVID-19 cases are dropping overall and reopening is underway, although millions of adults choose to...
COVID-19 News COVID-19 Resources COVID-19 FAQs
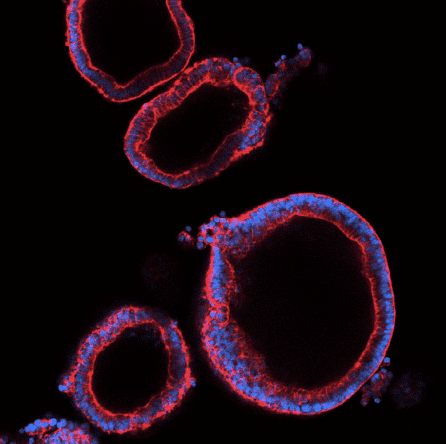
NYSCF’s chief goal is accelerating COVID-19 research by creating stem cell models for the scientific community that will enable studies of how the virus affects human cells and the discovery of therapies that can stop it. We are pursuing this by converting stem cells into the lung cells and other cells that are infected by the virus and responsible for the body’s reaction to the infection.
This approach is exactly what we use for researching the other major diseases of our time: creating patient-specific stem cells from blood or skin samples with the NYSCF Global Stem Cell Array®, and converting these stem cells into the cells affected by disease. Our COVID-19 research also benefits from our extensive, genetically diverse biobank of stem cell lines representing people with hundreds of underlying conditions that may influence their response to the virus.
We are now optimizing the ‘recipes’ and methods for converting human stem cells into lung cells that are susceptible to SARS-CoV-2 infection, to accelerate studies of how the virus infects and affects lung cells, how genetics may make certain individuals more vulnerable to severe cases of the disease, and to test therapies with the potential to stop or prevent infection. We are collaborating with experts in virology and drug discovery who will leverage our cell models for these purposes. To clarify the role of genetics in individual responses to the infection, we are using CRISPR gene editing technology in our stem cell models to introduce or correct the genetic mutations suspected of leading to severe cases.
At NYSCF, we are also applying our 3D printing technology to manufacture personal protective equipment for healthcare workers in New York City hospitals.

Numerous members of the global NYSCF Innovator community have pivoted their research to address this crisis community are now applying their expertise to address this crisis in a variety of ways, ranging, ranging from advancing the understanding of the disease, to facilitating rapid diagnosis, to identifying new drugs.
You can read more about the broader NYSCF’s community’s fight against COVID-19 here.
In the United States, COVID-19 cases are dropping overall and reopening is underway, although millions of adults choose to...
Watch the Fireside Chat video and read the summary below. After a historic research effort, COVID-19 vaccines are already...
Watch the Fireside Chat video and read the summary below. We are in something of a race between COVID-19 vaccines and...
The new coronavirus (COVID-19) is an infectious respiratory disease that has resulted in a global pandemic. The disease results from infection with the SARS-CoV-2 virus and can cause symptoms such as fever, cough, extreme fatigue, and loss of smell or taste. In some patients, the infection leads to severe, life-threatening respiratory distress. As of March 2021, there have been more than 500,000 deaths due to COVID-19 in the United States alone.
Individuals with underlying conditions like respiratory issues, heart disease, and diabetes, seem especially vulnerable — but some individuals who are otherwise healthy develop severe cases, which may be a function of their genetics. In most cases, the immune cells in our body will recognize and clear the virus relatively easily, but in severe cases, an aggressive inflammatory response known as a ‘cytokine storm’ is triggered that ends up attacking the lungs and multiple organs. Scientists suspect that certain genetic mutations may make individuals more likely to trigger this life-threatening version of the immune response. NYSCF is part of the COVID-19 Genomics Research Network in New York City, a multi-institutional collaboration applying advanced genetic technologies and data analysis to understand the role of genetics in how individuals respond to SARS-CoV-2 infection. Any genetic mutations identified that are associated with more severe cases can readily be investigated and validated in our stem cell models (see below). This can help us on the road to predicting who is vulnerable to developing severe COVID-19, and to find better ways to treat them.
If we are to fully understand and properly treat this disease, we need laboratory disease models that show us exactly how the virus affects our bodies. The most commonly used disease models are: 1) traditional cell lines, which require manipulation to allow infection and do not reflect the immune response; 2) mouse models, whose equivalent virus ‘doorway’ does not let SARS-CoV-2 into their cells; and 3) ferret models, who show a very mild response to SARS-CoV-2 infection. Stem cells, on the other hand, can be easily generated from anyone’s blood or skin samples using NYSCF’s world-leading technology, and converted into the specific types of lung and immune cells involved in COVID-19. Stem cell models of COVID-19 also offer the advantage of being genetically identical to the person from whom they are made, giving us a basis to study what makes certain people vulnerable to severe cases of the disease. We can study how different individuals’ lungs respond to the virus in a laboratory dish, without disrupting the patients.
Scientific collaboration is happening at a pace we have never seen before. Collaboration has been core to NYSCF’s approach since day 1, as progress is slowed by silos, but accelerated when experts pool their resources and perspective. At NYSCF, we are making these stem cell models of COVID-19 available to the entire research community so that they can be used for a range of applications in understanding and treating the disease. We are already collaborating with several leading virologists and chemists across the globe who plan to use our COVID-19 models in their research, including:
“This pandemic is devastating, but it has also brought about the most collaborative period of science that I’ve ever experienced,” noted MIT’s Feng Zhang, PhD, pioneer of CRISPR gene editing technology and NYSCF — Robertson Investigator Alumnus, during a recent webinar hosted by NYSCF. “I’ve probably met more people in the last four weeks than I typically would in a year, and everyone who I’ve reached out to about collaborating has been receptive. I think that speaks to how united we are in this fight.